As part of my work here, I am regularly confronted with desperately ill individuals who have seen dozens of physicians over the course of many years only to have their health continue to decline. Among the more frustrating aspects of this work is the failure of these physicians to assess and address the most basic aspects of health and healing. Namely, they fail to ask what the body needs to be healthy and whether the patient is getting those things. Of course, since evaluating these aspects health comes down to nutrition and exercise it does not align well with the practice of medicine, and if we are honest with ourselves, it is not something many of us want to deal with either. We want to eat what we want to eat and do what we want to do without regard to our health. Conventional medicine has capitalized on those sentiments, arguing persuasively for decades that a disease process is not real if all it requires to resolve is nutrients. Real illness requires medication, we now believe, having forgotten the very real nutrient deficient scourges like beriberi, Wernicke’s, pellagra, rickets, scurvy, and such.
Like most physicians, we have bought into the corresponding notions that fortification of foodstuffs assures that nutrient requirements are met and that in the land of plenty, where obesity reigns, malnutrition is rare. Neither is true of course, but belief in those myths absolves us of looking more closely at the chemistry of health and disease. For when we look at that chemistry, when we follow each of the altered signal transduction pathways, when look at the various patterns of deranged protein expression, and the myriad of genetic and epigenetic markers, we inevitably land at starving, inefficient mitochondria and the simple truth that they require nutrients to function; nutrient requirements that cannot be met by fortification alone and nutrient requirements, that if not met, lead to disease. When we dig a little deeper, we are also faced with a rather inconvenient truth that not only will pharmaceuticals not recover these deficiencies but they damage the mitochondria further. This does not accord well with the practice of conventional medicine and certainly does not fit into our busy, convenience-based lifestyles.
The Capacity to Survive
Among the more remarkable aspects of human physiology, however, is the capacity to survive all manner of illnesses and insults. We are supremely adept at adapting and surviving. We may not be living healthy, but we live. Mitochondria mediate these survival functions. They are responsible for converting the foods we consume and the oxygen we breathe into cellular energy (ATP). With that energy, they regulate all aspects of basic survival at the molecular level, including survival itself – cellular respiration – but also things like inflammation, immune function, steroid hormone production, cellular life and death cycles, and whole bunch of other stuff. As one might expect, each of these functions is energy dependent.
Decrements in cellular energy, thus, elicit those survival mechanisms. If they are not resolved appropriately, when the threat persists, and/or when there is limited energy to face the threat, these normal responses lead to all sorts of tissue and organ dysfunction. It is this mismatch between the energy available and the energy required that leads to the persistence of not only the original illness, but because of the chronically activated survival cascades, leads to new and more complicated illnesses. On the one hand, decrements in ATP lead to things like inflammation and immune system activation – the normal, programmed and encoded survival cascades – but on the other hand, the survival cascades themselves lead to decrements in ATP, which in turn leads to more inflammation and immune reactivity. Without resolution, these cascades can easily become ingrained and ultimately lead to death. This suggests that energy availability is the key to health, or more specifically, that insufficient mitochondrial energy, and thus, impaired mitochondrial function leads to illness.
From Power Plant to Battleship: Mitochondrial Healing Cycles and the Necessity of Sufficient ATP
A recent paper suggests this is true. Just last month, one of the leading experts in mitochondrial function, put forth a compelling synthesis of research delineating what he called the mitochondrial healing cycles. Specifically, he demonstrated by what systems level mechanisms mitochondria maintain health or initiate and maintain disease. Dr. Naviaux argues that chronic illness is initiated by the “biological reaction to an injury and not the initial injury or the agent of injury itself.” He uses melanoma as an example, illustrating how it is not caused by the sun per se, but our biological, or more specifically, our metabolic (mitochondrial) response, to the sun. Chronic illness, he argues, becomes chronic only when there is incomplete healing of the original injury and/or when secondary injuries occur before primary injuries have healed. Illness, he suggests, is a multi-hit proposition.
To Naviaux, illness begins and ends in the mitochondria. Mitochondria are responsible for enacting what he terms the ‘cell danger response’ (CDR), the survival mechanisms that I spoke of earlier. There are three phases of the CDR:
- The initial inflammatory/immune response: “activation of innate immunity, intruder and toxin detection and removal, damage control, and containment.” He aptly describes this phase as a shift in mitochondrial energetics and function from power plant to battleship. ATP has to be diverted to fight the threat, initiate and maintain the characteristic inflammatory response. The reduction in ATP results in the characteristic fatigue we all experience at the beginning of an illness.
- Once the damage from the initial injury is contained, phase 2 begins. This involves replacing the dead and damaged cells as well as walling off any remaining damaged tissue that was not completely cleared in phase 1. Here stem cells are recruited and enter the cell cycle. Mitochondria in stem cells are critical for this phase, supplying the stem cells with ATP as well as key substrates to help with healing process. An interesting aspect of this phase, is that cell – cell communication ceases. There is no metabolic cooperation between cells as they are continuing grow and migrate. It is only when growth is complete and migration ceases that cell-cell communication reemerges.
- In phase 3, we get a return to “cell differentiation, tissue remodeling, adaptive immunity, detoxification, metabolic memory, sensory and pain modulation and sleep tuning”. Once the cells have been fully differentiated and re-educated, cell-cell communication reinstates and healing is complete.
The healing cycles are linear, sequential and ATP intensive. Each must be completed before the next can begin, before a secondary injury takes place, and each requires a continuous supply of ATP. Too many hits and/or too little ATP will derail healing. When we consider mitochondrial metabolism as the root cause of persistent disease, it is difficult not to ask what constrains the availability of energy and thus blocks the body’s ability to progress across each healing cycle.
Recovering Mitochondria: The Role of Nutrition
To answer this question, one has to look at how we produce ATP. Absent outright starvation, to get from food to ATP we need a few things: macronutrients and micronutrients or proteins, fats and carbohydrates along with vitamins and minerals. That’s it. Nothing fancy or complicated, just basic nutrition.
When we look at macronutrient consumption, one of the leading problems in western cultures is the high consumption of junk, carbohydrate-based foods. These foods, though they are often fortified with vitamins and minerals, come with far more sugar and other toxicants than the body can handle. Rather than being a net gain in energy, ultimately, become a net loss, both in macro, but especially, in micronutrients. Without sufficient micronutrients, none of the enzyme machinery, whether in the cytosol of the cell or in the mitochondria themselves, can perform the required functions that moves the macronutrient through the factory and produces ATP. Indeed, even the consumption of molecular oxygen requires the presence of vitamins and minerals. Absent those vitamins and minerals, a sort of cellular hypoxia sets in; one that activates inflammatory pathways, and ultimately, the shift in tale tell shift energy production associated with cancer known as the Warburg effect.
Conversely, because of decades-long advertising campaigns, most folks, but women especially, consume insufficient quantities of protein and fat. This skewed consumption of macronutrients places a high demand on the OXPHOS (oxidative phosphorylation) pathway of the mitochondria to produce ATP, while simultaneously not providing sufficient micronutrients to fuel the enzyme machinery to produce this ATP. It also increases the need for detox, while again, failing to provide adequate substrates to do. Moreover, if the diet is high in the staple sweetener high fructose corn syrup, in addition to everything else that becomes dysregulated at the mitochondrial level, the ability to covert fatty acids into energy, can be shut down entirely, conferring a metabolic inflexibility that is common in western cultures.
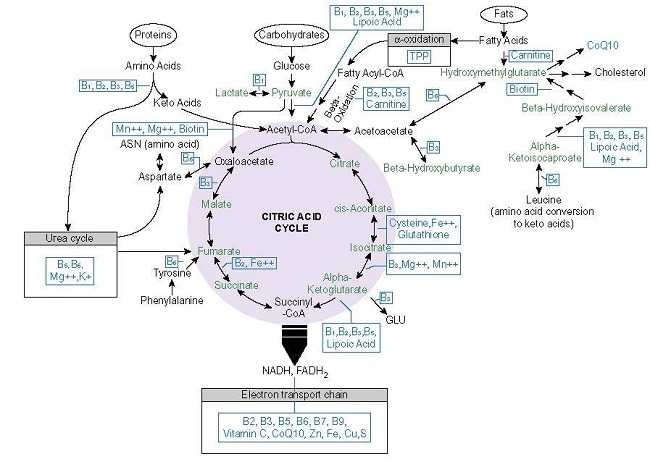
Along with issues with macronutrient consumption, large percentages of the population are deficient in one or more of the micronutrients required for healthy mitochondria. Individuals with chronic illness are severely deficient. The mitochondria require 22 vitamins and minerals in varying concentrations to convert the food we eat and the air we breathe into cellular energy or ATP (Figure 1.). Absent sufficient concentrations of one or more of those nutrients, mitochondrial function deteriorates and healing will not progress. Survival mode is all that can maintained.
With Naviaux’s framework, it becomes clear that healing is an energy intensive process. The only way to boost energy is via good nutrition. Sure there are compounds that can override certain pathways within the mitochondria and, at least temporarily, provide additional energy, but if the core requirements for optimal mitochondrial health are not met, it is only a matter of time before initial benefits become problematic. (I should note that exercise is also critical for healing the mitochondria. Exercise forces mitochondrial biogenesis among other important processes.) The questions that physicians and individuals with chronic illness should be asking are:
- What is required for health?
- Is this patient or am I getting those things?
Unless and until those aspects of health are addressed, chronic illness will persist because the mitochondria simply do not have the resources to progress through the healing cycles. There are no short cuts here.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image credit: ImgFlip, Template ID: 24838763
This article was published originally on October 17, 2018.