The use of the word model is supposed to describe the nature of disease as it differs from that of health. Hippocrates was the first person to offer a solution to the preservation of health by saying “Let food be your medicine and let medicine be your food”. Throughout most of history there was no model and treatment was based on largely futile ideas. The present age of medical thinking was ushered in by the discovery of disease producing microorganisms. The model became “kill the microorganism, the bacterium, the virus, the cancer cell”. If no microorganism or cancer cells could be found, the remaining diseases were long considered to be a mystery.
Recent research has advanced the model by discovering that the brain controls inflammation through the vagus nerve by the use of metabolites called cytokines. However, the present medical model still dictates that the various symptoms that signify loss of health are put together in collections. Each is considered to represent a particular disease that has to be named for diagnostic purposes and that a cure for each is to be found from detailed research. So we now have literally thousands of different diseases, often being called after the person who first observed a particular symptom/sign collection, such as Parkinson or Alzheimer. Each of the named diseases is supposedly recognized by a collection of laboratory tests that are “diagnostic”. What is even worse, is that this collection is often called a syndrome and the first observer has his/her name appended. From that time on, this particular collection is known as “Joe Soap’s syndrome”. Fortunately, there is change on the horizon as we gradually realize that the human body is a “machine” whose function is metabolic in nature.
The Stress of Life
When I was in active practice, I discovered that thiamine could be used as a “drug” for many of the situations that I encountered, seemingly irrelevant to the diagnostic category with which I was supposedly dealing. I was thought of by my colleagues as a medical heretic. Since it had long been known that thiamine deficiency was responsible for the disease called beriberi, I studied the history of the early attempts to find its cause. Beriberi had existed for thousands of years and was still largely a mystery at the end of the 19th century. I found how easy it was for the investigators to be misled. In Eastern cultures rice had been a staple for centuries. At that time, factories had been built in China in which buildings had been separated by a corridor. In the summer months the workers would congregate in them to take their lunch. As the sun moved around, it would shine on the congregated workers and several of them would come down simultaneously with the first symptoms of beriberi. The obvious conclusion for the investigators was that this was some kind of infection since several of them had succumbed at the same time. When it was found that thiamine deficiency was responsible, an explanation was required for this simultaneous incidence of the disease.
We now know that ultraviolet light is a source of stress. It can be concluded that the affected workers had been marginally deficient in thiamine. They were either asymptomatic or had mild symptoms attributed to other causes. The stress caused by sunlight had provoked symptoms of the disease simply because the required energy was unavailable to achieve homeostasis. This intriguing discovery caused me to seek the work of Hans Selye, whom I visited in Canada. As I have written in several posts on this website, he had determined from the study of rats that each form of stress had to be resisted and required energy. He called it the General Adaptation Syndrome (GAS) and offered the idea that human disease was a lack of sufficient energy required for adapting to the more severe environmental influences encountered on a daily basis. This included severe trauma and infections. The energy deficiency conclusion of Selye was later backed up by one of his students who was able to produce the GAS experimentally in a thiamine deficient rat without using any form of experimental stress.
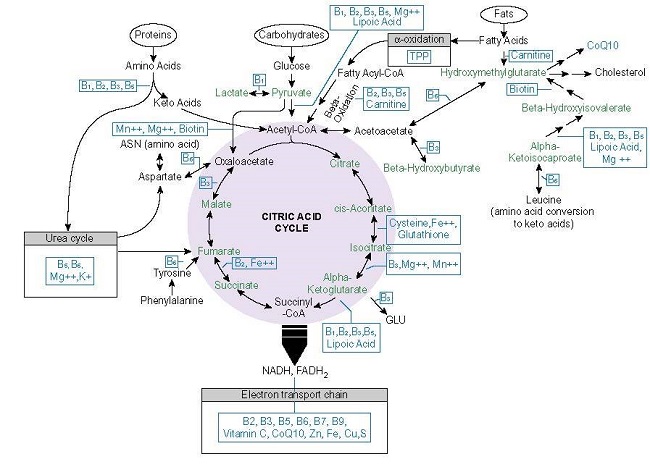
It seemed to me to be obvious that I had to study the way energy is produced in the human body if I were to understand the reality of health and disease. In Selye’s time energy metabolism was poorly understood and it was a mark of his genius that enabled him to suggest that it was energy deficiency that caused the collapse of the GAS. The reason that all animals, including humans, are living is because they construct energy from food and this creates a chemical called adenosine triphosphate (ATP). From there, electrical energy has to be created and that is the energy that we use for functional activity. The transition from chemical to electrical energy is not precisely known but there is some evidence that thiamine in the form of thiamine triphosphate (note the parallel with ATP) plays an important part. This triphosphate form is exceptionally high in the electric organ of the electric eel, capable of producing a paralyzing shot of electrostatic electricity to zap its prey. The electric organ is an adaptation of a nerve ending just like ours. It is obviously important to understand that this is an evolutional adaptation and does not mean that we can produce a high energy output from our nerve endings. Indeed, the evidence is strongly in favor of the energy being in microvolts. We are identifying the electrical potential when we perform an electroencephalogram or an electrocardiogram and a recent test has been devised using the electrical potential of a person with Chronic Fatigue Syndrome (Open Medicine Foundation April 2, 2021).
Many of the people reading the information on this website are themselves patients seeking help for their misunderstood disease. The history recorded in their posts is repetitive and in each case their reported symptoms are usually thought to be bizarre by the physicians that have been consulted. In the present medical model a “real” disease is called organic and is marked by a series of abnormal laboratory tests. When these tests are reported to be normal, the conclusion is nearly always the same. The symptoms are considered to be imaginary in a person who is thought to be psychologically abnormal. They are referred to as psychosomatic and the patient is told that “it is all in your head”. It is always surprising to me that the physician seems to have the belief that the bizarre nature of the symptoms is generated in the patient’s brain without consumption of energy, that thought processes or imagination are not the result of energy consumption by brain cells.
Distorted Truth
The real trouble is that the disease model represents a distortion of the truth. To make a diagnosis, it is inherently necessary that some of the presently used laboratory tests must be abnormal. No thought is given to the possibility that energy deficiency in the brain might be the cause of the symptoms. Therefore no effort is made to obtain the right laboratory tests. It demands a totally different way of thinking about health and disease. People affected by this kind of brain energy deficiency disease are often working and living ostensibly normal lives but suffering greatly. They are in fact experiencing early beriberi, a disease that has a long morbidity and a low mortality. They can go on experiencing these symptoms for years, but if they are completely ignored as psychological misfits, one can easily imagine that permanent damage will develop. Perhaps Alzheimer’s and Parkinson’s disease are really reflections of this permanent damage and that there will never be a “cure” for them. Attention to relatively simple symptoms, usually diagnosed and treated as variable named conditions such as “allergy” may be the only way in which these named diseases can be prevented.
To give an example of this kind of thinking, I was confronted by a 12-year-old African-American girl with extremely severe asthma occurring in individual attacks. Physical examination revealed that her body was covered with “goose bumps”. Because of this I came to the conclusion that her autonomic nervous system was dysfunctional and the cause of her asthma. I had already come to the conclusion that thiamine deficiency caused the energy failure that resulted in dysautonomia and that sympathetic/parasympathetic imbalance could affect the bronchial tubes. Without further testing, I gave her thiamine in pharmacological doses. It resulted in a complete disappearance of the asthma. This patient, at the age of 30 years, contacted me to let me know that she had only experienced two mild attacks of asthma in her 20s.
Health Requires Energy
What is important to remember is that any situation involving physical or prolonged mental stress requires energy in the brain, used to organize the complex defenses of the body. The recent discovery by Dr. Marrs and myself that thiamine deficiency in America is common, suggests that brain energy is insufficient in many people. If and when they are attacked by a microorganism such as Covid-19 it is possible their symptoms and their continuation reflect brain energy deficiency. Consequently perhaps they are unable to adapt and overcome the stress of the viral attack. It also suggests that symptoms expressed by so called Longhaulers might be helped by the administration of pharmacological doses of thiamine.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on April 7, 2021.
Image by Joshua Nicholas Vanhaltren from Pixabay.