Ever since I learned about connections between trehalose, the synthetic sugar now pumped into all food products (Figure 1.), and virulent infections, I could not help wondering if there were not some additional connections to be made; namely between our consumption of trehalose-laden products and the explosion in insect-borne illnesses over the last few decades. Illnesses of the tick-borne variety have become especially common here in the US, but mosquito carried illnesses seem also to be on the rise. In just a few decades, the incidence of Lyme disease has more than doubled and while we don’t talk about mosquito or other insect-borne illnesses as much in developed countries, a peek at the data suggests rates of these illnesses have tripled between 2004-2017.
Among the reasons cited for the increase in insect-borne illnesses, climate change is top among them. Shorter winters, and longer and warmer summers increase the breeding and survival capacity of the insects, their pathogens, and the animals that harbor and transport them. On the surface, this gives us little actionable information and often unleashes a political hailstorm of useless rhetoric. When we dig a little deeper, however, this may be a very important clue. For what is at the root of climate change is also at the root of a whole host of other problems, including possibly, the increase in insect-borne illnesses. It is none other than our decades-long love affair with synthetic chemicals. The chemicals we have dumped into the atmosphere, waterways, and soil and into and onto our bodies are causing a wholesale change in environmental and organismal metabolism. These chemicals impair mitochondrial functioning, diminish energy capacity and with that, reduce our ability to effectively meet the demands of living. So, when infection strikes, we are unable to clear it.
Metabolic Hypoxia
From a molecular standpoint, the constant exposure to synthetic chemicals causes a sort of functional hypoxia, for us and every other biological organism. It’s not a choking, obstructed airway kind of hypoxia, not yet anyway. It is a metabolic or cellular hypoxia that initiates slight perturbations in cellular functioning that accrue over time. Our cells breathe. They, or more specifically, the mitochondria within the cells, take the oxygen from the air we breathe and along with some nutrients convert this into usable energy. When damaged by synthetic chemicals and/or absent the nutrients, it does not matter how well we breathe, and chances are we do not breathe that well – think apnea – that oxygen cannot be used effectively. When that oxygen cannot be used, the cells become hypoxic and start sending out signals far and wide meant to mobilize more oxygen. These are meant to be short-term, stopgap survival measures until the toxicants are cleared and the nutrient-fueled enzymes kick everything back into gear. Increasingly, however, this does not happen since everything we consume or are exposed to comes with an unhealthy dose of toxic crude and few of us consume sufficient nutrients to compensate.
What does this have to do with the increase in insect-borne illnesses? Everything. Just like us, when faced with unhealthy ecosystems, the insects and the microbes they carry enact adaptive mechanisms geared toward survival, mechanisms that ultimately favor increased virulence. Virulence from the insect’s/microbe’s perspective, if it were to have one, is nothing more than survival, the same survival we cling to, and the mechanisms, though slightly different in specifics, hold broadly to the same principles. Molecular hypoxia, the kind that develops from nutrient deficiency, is a stressor that demands survival cascades. For us, this involves inflammation, immune system re-regulation, and a myriad of molecular mechanisms designed to increase oxygen delivery and usage; think metabolic, autoimmune, cancers, and the other chronic illnesses that are endemic, including those of the insect variety. What is interesting though, is that for insects and microbes, including the microbes in our gut, the survival cascades involve the synthesis of a specific fuel that is used only as a last resort. And you guessed it, that fuel is trehalose.
It just so happens that from the year 2000 onward, we have been mass producing and consuming trehalose, the survival fuel of preference for insects, fungi, bacteria, and viruses. This is a boon for insects and microbes, but not so good for us. Before 2000, most of us would have rarely consumed trehalose and it is not something we synthesize endogenously to any great capacity. Sure the bacteria in our gut will synthesize this fuel but minimally compared to how much we consume these days (many grams or more, the data are lacking), and only when severely stressed. I have written about this sugar previously, here and here, but its likely relationship with the proliferation of insect-borne illnesses necessitates another look. Oh, and as you might expect, there is a thiamine connection.
Figure 1. Trehalose in Food Products
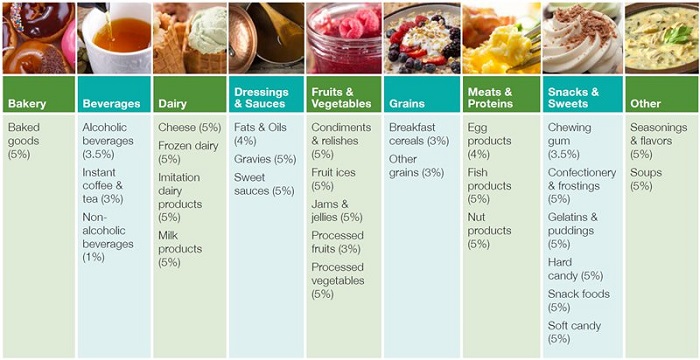
According to the company website: “TREHA™ trehalose can be incorporated into a wide variety of applications and is GRAS [generally accepted as safe] up to the use levels specified” above. In other words, these products can be composed of up to 5% trehalose. (Note, since originally publishing this article in 2019, the company has removed the page with this table.)
Trehalose, Thiamine, and Survival
All organisms, including the microorganisms that line every surface of our bodies and those in our gut, require thiamine (vitamin B1) to produce energy. Absent thiamine, fungi, bacteria, viruses (and insects, invertebrates, and plants), adopt secondary survival pathways using ‘rescue’ sugars for energy. The use of these rescue sugars bypasses the thiamine-dependent oxidative phosphorylation pathway. Trehalose is one of the primary rescue sugars used by microorganisms to withstand severe environmental stressors like desiccation, dehydration, heat, cold and oxidation, and a basic lack of nutrients. During times of stress, trehalose is synthesized de novo (from scratch) by most microbes. Though a simple sugar used for energy production, trehalose is essentially a preservative. It preserves the integrity of cells when nutrients are absent, hence its ability to withstand desiccation and dehydration.
In 2000, for the first time in history, trehalose was commercially produced and sold as a food additive by the chemical company Cargill. Since then, it has found its way into all types of processed foods as a sugar additive, a salt-substitute, and a preservative. It has even been bandied about as a healthy supplement for kids with Autism. From the company website:
“Trehalose is an ideal ingredient for generating exciting market possibilities for your latest product concepts and also for adding new life to existing food and beverage brands. Trehalose, a diglucose sugar found in nature, confers to certain plant and animal cells the ability to survive dehydration for decades and to restore activity soon after rehydration.
This observation has led to the use of trehalose as excipient during freeze drying of a variety of products in the pharmaceutical industry and as an ingredient for dried, baked and processed food, as well as a non-toxic cryoprotectant of vaccines and organs for surgical transplants.
It is especially well suited for sweetening nutritional drinks and other energy products used by consumers as part of their daily eating habits. As a multi-functional sugar with nearly half the sweetness of sucrose, trehalose will strongly improve the taste, texture, and appeal of your foods and beverages. Trehalose can bring out the best in your products and your processes, enhancing functionality and improving stability in several key ways.”
The downside of this wonder sugar substitute is precisely its claim to fame. It is a survival sugar. It helps microbes survive; the good ones, but most especially, the bad ones. Just last year we learned that the addition of trehalose to commercial foods is linked to the rise in treatment-resistant Clostridium difficile (c-diff). I would argue that it is also linked to the rise in glabrata infections, a nearly intractable yeast infection. Indeed, one test to determine glabrata relies on its ability to identify trehalose in the specimen. Research shows a connection to intractable tuberculosis and I suspect also that trehalose is involved with the increasing number of foodborne outbreaks in listeria, salmonella, and e coli infections.
As a survival sugar, the adaptability of organisms to activate the trehalose pathway confers virulence – survivability, even in the face of strong antibiotics. It should be no great surprise then, that when consumed in great quantities, it does just that. The question is why do only the ‘bad’ microbes seem to benefit? Wouldn’t all microorganisms benefit equally from trehalose? Perhaps not. The researchers in the C-diff study suggested that trehalose differentially affects microbe survivability and that only the most virulent and the strongest survive. They found that the most virulent strains under stress (starvation for cell culture) were able to mutate in a particular manner that allowed them to transport and metabolize more trehalose than the less virulent species of the bacteria. The mutation that developed, unregulated an enzyme involved in the trehalose to glucose conversion pathway (trehalose 6 phosphate synthase – tps1). From other research, we know that this particular enzyme is thiamine-dependent. In this case, the enzyme upregulates when thiamine is depleted.
Arguably then, host thiamine deficiency alone, absent a ready supply of exogenous trehalose, contributes greatly to the increase in highly virulent, treatment-resistant infections that we have seen over the last few decades. Standard treatment protocols which involve antibacterials, antifungals, and the like, exacerbate thiamine deficiency further by the damage done to the mitochondria. This then leads to and reinforces treatment resistance by upregulating microbial trehalose production. It is a vicious cycle.
Low Thiamine Plus Dietary Trehalose?
We know from research with plants, that thiamine does more than just divert energy synthesis away from the trehalose pathway. Thiamine signals a myriad of protective pathways to prevent pathogens from gaining a foothold in the first place. It is an immune reaction of sorts. Interestingly, thiamine not only confers a quicker response, it seems to induce a future resistance towards that pathogen. That means that thiamine elicits a faster, stronger, and longer lasting immune response, than compared to conventional antimicrobials, but it also primes or trains the immune system conferring future resistance. Of course, this is in plants, but it suggests we may be going about fighting these infections all wrong. Perhaps rather than attempting to kill everything, we ought to be bolstering host defenses.
Returning to the problem of dietary trehalose, the question remains: what happens when we combine a thiamine deficient host and a diet packed with trehalose? The modern diet is such that even without the addition of trehalose to foods, many folks exist in a state of nutritional deficiency. The trehalose only adds to these deficiencies, providing nothing more than empty calories. That alone is problematic, but because of its unique role as a microbial rescue sugar, we are now bolstering the survivability of pathogenic microbes by providing them with a ready and continuous fuel source while simultaneously starving the host of critical nutrients. It is a double hit that confers virulence, with the diet of the host as much or more responsible for the virulence of the insect-borne pathogens. One could argue based on the chemistry that the mutations in the microbes that lead to pathogenesis are controlled, not by some unique mechanism of the bacteria, but by the interaction with the host’s nutrient status.
Returning to insect-borne illnesses, are these dietary changes making us more attractive to the biting insects like ticks or mosquitoes, and once bitten, could the lack of thiamine paired with the ready supply of trehalose maximize the growth potential of the pathogens carried by these bugs? The research on this is circumstantial at best. We know that both the tick and the bacteria that lead to Lyme disease both use trehalose. Additionally, we know that ticks and mosquitoes are attracted to both excessively high and low concentrations of lactic acid – characteristics of low thiamine and that thiamine is used prophylactically to repel insects, though the research is limited and contradictory. Perhaps thiamine does not repel insect bites as suggested anecdotally, but rather, bolsters the host’s immune system such that it is capable of clearing any potential pathogenic infections.
Interestingly, unlike every other bacterial organism, the Lyme bacteria Borrelia burgdorferi does not appear to require thiamine to survive. Does that mean that it will survive independently of host thiamine status? Maybe. Although I suspect that as with the plant research mentioned above, host thiamine status affects the strength of the immune response to the pathogen. I also cannot help but wonder if the lack of thiamine response in the Borrelia bacteria is not some recent evolutionary adaptation to trehalose availability. Remember, trehalose is the survival sugar of choice, whose synthesis is upregulated in the absence of thiamine. Twenty years of trehalose availability for insects and microbes is akin to a millennium in larger organisms – long enough to induce genetic and certainly epigenetic changes. If this is the case, the explosion in Lyme disease is only the tip of the iceberg.
Although these connections are purely hypothetical at the moment, with little direct research to prove causation, the patterns and chemistry fit. At the very least, there is sufficient circumstantial evidence to warrant exploration. For individuals struggling with insect-borne illnesses like Lyme disease and/or with intestinal manifestations of an altered microbiome, avoiding trehalose products and maximizing nutrient intake may make all the difference in fighting these infections.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on May 28, 2019.
















I’m desperate for some sort of direction. I got bit by what was told a brown recluse bite in 2003 in the Army. Deployed a year later to Iraq, intense combat for months. Developed neck pain and headaches frequently over there. Lost my gallbladder shortly after the army in 2007. In 2020 I attended a tbi clinic for military post concussion issues. My hormones were out of wack and I had frequent anxiety/ fight or flight. I was put on some supplements, testosterone cream and low dose naltrexone. About 3 months into the LDN I was feeling great. Felt very normal for the first time in years. Then when I upped my dose, I started getting weird symptoms. Extreme fatigue, diarrhea, shakey, nausea, and more. My resting pulse fluctuates from 80-115, elevated bp. I stopped the LDN and slowly started feeling a little better but had frequent fight or flight. My doctor tested me for some infections and came back positive for mycoplasma pneumonia, Lyme, bartonella, and others.
Initially I was put on azithromycin for 4 months but couldn’t get past 3 weeks. It wrecked my stomach and nauseous. I was afraid to try anything else and then started getting vertigo a month after I stopped. I went to the hospital and was given some meclizine and muscle relaxers. I felt better for a short time. I then developed dizziness when I stand up. I went to another tbi clinic in Boston and they referred me to Neurology at Mass General. They diagnosed me with PPPD. They didn’t want to hear about Lyme or potential nutrient deficiencies.
I also tested positive for multiple mycotoxins. I’ve essentially been house bound for 2 years. I have children and cannot keep making my family suffering. I’m about to do some more blood work. Full hormone, nutrients, tick 2.0 vibrant panel, and organic acids test (urine). Is there anything else you’d recommend?
I suspect given all of the stressors you experienced, the bite, the combat, the medications, and life in general, that you are extremely depleted in mitochondrial capacity to produce ATP. The only way to fix that it is to begin providing the mitochondria with what they need to convert the food you eat into ATP/energy – micronutrients – vitamins and minerals. Begin with thiamine, magnesium – we have lots of articles on the topic and wrote a book (listed on the website) about what happens when these nutrients are subpar. Everything goes wrong. Take a look, I suspect you will see your symptoms expressed clearly in these deficiencies. If you would like to write up and allow me to publish your full case story and perhaps get more insight from me and other who will read it, let me know. In the mean time though, read everything you can on thiamine deficiency from this site and others and look on youtube for videos. There are many.
So Trehalose is in vaccines also as a preservative. I wonder if this is linked to long covid and other autoimmune conditions linked to the vaccine
This just seems like more proof that we’re meant to eat an animal based diet as humans. Considering the awful disease obtained by certain tick bites that causes a person to become nauseated by meat ingestion, it totally makes sense evolutionarily speaking that a bug would have an advantage by inducing this in a human which would force more consumption of low thiamine food sources. At the very least, we should aim to consume only whole natural foods and only vegetables and fruits in season locally. Great article and I think I will help many clients with this information. Thank you!
Maybe I missed it but is there a max amount we should be trying our consumption to? All those foods listed are considered high and we should avoid them?
I’m quite concerned to learn this. I’m currently undergoing a long and expensive FMT protocol with a leading clinic in Australia, their protocol is followed by gastroenterologists worldwide. The FMT infusions are made with trehalose. And the antibiotics and antifungals I took in preparation I’m quite sure damaged my mitochondria further. Suddenly feeling backed into a corner. Is the path out going to be thiamine repletion?
I had no idea trehalose was used in FMT. That could be one of the many reasons folks have negative reactions to FMT. Thiamine is certainly an option, perhaps even the answer, along with the repletion of other nutrients.
Chandler,
I cannot believe I opened hormonesmatter tonight to learn this.
As many may know, I was chronically thiamine deficient (TD), now dependent. My story’s published here.
For the first time since 2018, I felt up to a 7 hour trip from Rhode Island to stay at a friends house on a lake in Caribou, Maine.
I “crashed” returning home from that Memorial Day 4 day trip. For two weeks, I was down. I noted 5 mosquito bites on my lower right leg, photographed them and told my daughter I felt like “I caught something in Maine,” telling her my concern about the bites and mosquito born illnesses. I thought, thankfully I was high dosing thiamine already, but had backed off my protocol “being away.” What usually takes me 3-5 days to return to my baseline, took two weeks and I’m still reeling with painful joints; nerve, muscle, and pain into my bones. My arms & legs tingle, pins & needles, and greater numbness in both arm’s especially. I’ve already been diagnosed with severe SFN (small fiber neuropathies) attributed to TD.
I was running a low grade temp the following week. I’m usually normally in the low 97 degree range. My BP shot up, I was tachycardic with a lower O2 saturation for me. My “pseudo hypoxia” symptoms returned a bit too. I’d been journaling x3 years, monitoring my vitals on my thiamine protocol journey.
I’ve slowly reupped my thiamine but as suspected, after reading THIS article, I understand better.
The stress of the trip, the lifting and stair climbing exhausted me, literally using up all my energy. I’ve been mostly bedridden again. The muscle weakness is far worse than ever. All my TD and SFN symptoms exacerbated!! I fell off my clean whole foods, no sugar low carb diet in Maine, then more so upon return, “stress eating.”
I added “FUEL to the fire,” quite literally; I see NOW, especially after reading this article.
I had no understanding of this type of sugar, TREHELOSE, surprisingly in all my researching. Once again, you’ve enlightened me and I am excited to share this information with my RN daughter who blew me off when I suspected my symptoms MAY be related to the mosquito bites!
Wish I could get tested to prove your theory but I AGREE wholeheartedly with it!!
Multiple factors more easily drain my thiamine, which after long term deficiency, is now my life. Any “stressor” crashes me. Fortunately, I’ve learned the importance of THIAMINE therapy to heal. It’s remarkable how it’s helping me regenerate nerves in my eyes and all over but this incident really knocked me down.
I’ll have to write more about this and share your article! THANK YOU ONCE AGAIN!!
You know Jane, Asa side effect of my beta blocker I have dry eyes.. guess what is in the eyedrops I have been using for this since months.. right… This nasty Sugar thing. The drops name is Thealoz!!!
Superb article, I had never heard of Trehalose before. I will watch out for it from now on. What would be nicer than all these clever chemicals would be if they stopped messing with the food.
It would be nice, wouldn’t it.
I am afraid that they don’t often list it in the ingredients, along with a number of other chemicals in processed foods. They often have very benign sounding names like all natural sweetener and such.