I first noticed symptoms of what I believe to be functional dysautonomia that affects my peripheral circulation in the winter when I was 12 years old. Though they have never completely derailed my life, like the symptoms of so many others, they are a constant presence. I am now 21 and the symptoms have more or less stayed the same since that winter.

These symptoms mainly impact the peripheral circulation on my hands, feet, and face. They are triggered, or worsen, when exposed to heat, cold, stress, or alcohol. Most of the time my hands and feet will have a slightly cyanotic tinge, are cold, and (feet especially) will sweat. When it is very cold they will turn to a bluish color. While standing still or when my hands are by my side they will get blood pooling in a bluish / purplish mottling color. In addition, my capillary refill time is very slow, especially on my feet, sometimes in excess of 12 seconds.

When it is warm my hands and feet will become red and hot, with blood pooling in them when placed below the heart, if I raise them they will return to a normal color. Also, when hot I will get prickly / itchy sensations on the back of my arms and on my back. My cheeks, in addition, are often quite red, even in a cool room, and get more so when I am hot or stressed. My brother also has these similar circulation issues.
Apart from these physical symptoms I noticed, I have dealt with fairly bad anxiety since I was young, especially around school and sports. It has gotten much better in the last year or so after I noticed it and worked through it. Through recognizing it, I realized how much of the time I was in a tense sympathetic state. Another random symptom I have had since I was young is eye floaters. I am not sure if the two are related. Other than those symptoms, I feel as though I am healthy. I am able to stay active and am studying in college.
It’s More Than Raynaud’s Syndrome
Every time I attempt to get these symptoms checked doctors say they can find nothing wrong with me and that it is either Raynaud’s or “just how it is”. Though, from my own research, it appears to me that is not the case. The only other examples of symptoms I can find like mine are pictures of POTS patients with dependent acrocyanosis / blood pooling in their arms and legs and a case study of Dr. Lonsdale’s of a girl with juvenile arthritis. I find my own symptoms confusing mainly due to the lack of other symptoms.
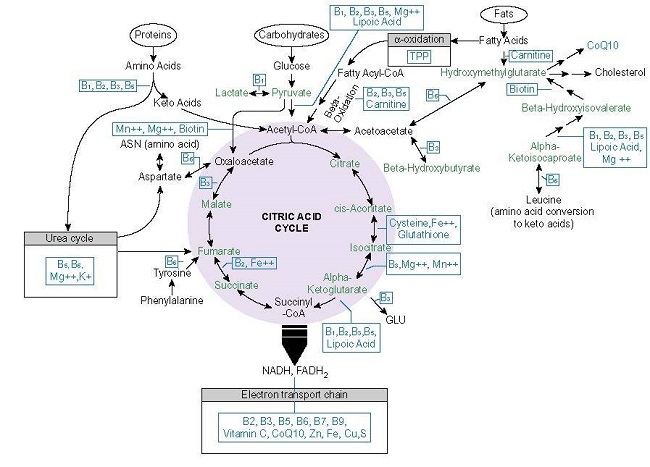
Perhaps Thiamine Will Help
After taking time reading through this site and looking through Dr. Lonsdale’s work, I started taking 50mg of Allithiamine and 125mg of magnesium daily, about a month ago. During this first week of taking it I noticed a twitching in my stomach, general stomach pain, and I would sneeze a ton. After a week, I bumped it up to 100mg of Allithiamine and 250mg of magnesium, during this period I noticed very intense dreaming, which was constant throughout the night, and an upset stomach. After a few days of this, I dropped magnesium down to 125mg and kept thiamine at 150mg. I am now at 200 mg of Allithiamine and 125mg of magnesium a day. It has been four weeks since starting Allithiamine and I have not experienced further strange symptoms, however, I have not noticed any of my main symptoms, the issues with peripheral circulation, reduce.
I am just curious if I am on the right path and if anyone would be willing to offer some guidance.
Thankful for This Community
I am so appreciative of this community. I cannot describe how grateful I am to have this paradigm for thinking about health at such an early age.
Thank you to everyone who took the time to read this, Dr. Lonsdale for all of his work, and Dr. Marrs for her work and encouraging me to post this.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.