Everything slows down as we age. For some lucky folks, aging happens gracefully with nary a disease in sight. For others, the springs start popping off around 40 and by the time we reach ‘old age’ our bodies and brains are barely functioning. Arguably, diet and lifestyle have something to do with how well or how poorly we age, and of course, genetics contribute mightily, but beyond that, we really have no idea what’s happening with aging.
Sure, there are all sorts of physiological systems that become progressively less efficient over time. Wear and tear plays a huge role, but the relationships aren’t linear. There are always outliers. There are folks who, on a diet of smokes and scotch, live well into their nineties with all their faculties intact. Then there are the poor souls who are prodigiously healthy, who eat right and exercise, but yet, whose bodies seem set on wide-scale destruction, where the slightest change in lifestyle risks sending them into a morass of cascading illness. Somewhere in the middle, the rest of us live – sometimes healthy, sometimes not – aging in fits and spurts. What the heck?
From a physiological standpoint, aging is marked by two opposing factors: decreasing hormones and increasing inflammation. Where they intersect, age-related illnesses seem to accrue. Called endocrine senescence, researchers have long noted a relationship between declining hormones and declining immune function (marked by increased and inefficient inflammatory responses). Might there be some truth to the ever-young, hormone peddlers? Could hormones be the key to offsetting the age-induced inflammatory cascades? Possibly.
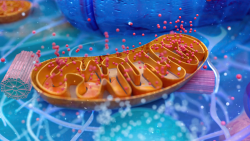
Hormones and Mitochondria
I just finished writing an extensive paper on acquired mitochondrial illness. Throughout the research, I stumbled upon a short essay linking mitochondrial structure and function to estradiol. More specifically, the rapid estradiol decline common post oophorectomy (ovary removal), fundamentally alters the shape, and ultimately, the function of mitochondria. Researchers found that a rapid decline in estradiol evokes significant damage in the brains (and presumably other organs) of female monkeys. Additional studies using estradiol starved mitochondria from female rodents showed similar shape alterations and consequent declines in brain bioenergetics. Interestingly though, with natural menopause, where estradiol declines more gradually, no such structural changes were observed. In fact, with the more gradual decline in estradiol, the mitochondria appear to increase their production of the lifesaving ATP as a compensatory reaction.
All Paths Lead to the Mitochondria
Recall, from previous posts, that mitochondria take dietary nutrients and oxygen, and change them into the chemical energy (ATP) that is used by every cell in the body. Without ATP, cell function grinds to a halt. So, anything that derails the mitochondria, imperils cell function and initiates cell death. Lack of nutrients, sedentary lifestyle, pharmaceutical, and environmental toxicants, all derail mitochondrial function. Cluster too much cell death together in one tissue or one organ and disease happens. Since mitochondria are in every cell of the body, mitochondrial damage induces disease broadly, but especially in regions with high energy demands like the brain, the heart, the muscles, and the GI system.
The cardinal symptoms of mitochondrial damage include fatigue, weakness, muscle pain, and depression. These are followed by dysregulated systems; a GI system, for example, that overreacts or under reacts or temperature dysregulation (hot flashes, cold insensitivity), insulin/sugar dysregulation, emotional volatility, migraines, seizures, syncope (fainting), and so on. It’s not a pretty picture.
In addition to providing the fuel for cellular respiration, e.g. life, mitochondria control a host of other functions, steroidogenesis is one of them. This means that if we fail to feed the mitochondria or hurl insults at them, hormone dysregulation is inevitable. Ditto for inflammation, as the mitochondria regulate inflammatory cascades. Every woman knows when her hormones are out of whack. Well, now we know that hormone dysregulation emerges from the mitochondria.
From a systems perspective, consider the mitochondria as central regulators of organismal health. Mitochondria both send and receive signals from all over the body and then adjust their functioning accordingly. With their role in hormone synthesis, we would expect there to be cross-talk between the mitochondria and circulating hormones. Indeed, there is. All steroid hormones have receptors on the mitochondrial membranes. When hormone concentrations increase or decrease, the mitochondria will initiate the synthesis of new hormones and send signals throughout the body to adjust other hormone-responsive systems as well.
No Estradiol Equals Misshapen Mitochondria: Donuts and Blobs
Removing the ovaries starves the mitochondria of one of its many feedback mechanisms and damages the brain mitochondria in the regions of the brain responsible for executive function and memory – the frontal cortex and the hippocampus. The mitochondria change shape, from spheres (healthy) to donuts and blobs, which represent early and late-stage mitochondrial damage, respectively. Misshapen mitochondria cannot provide the energy (ATP) needed to perform critical brain functions such as neural communication or the antioxidant tasks needed to clean up toxicants. Neurodegeneration ensues. In layman’s terms, and in the early stages, brain fog and memory loss. Researchers believe that it is this loss of functional mitochondria that contribute to the onset of neurodegenerative disorders like Alzheimer’s and other dementias. And, this loss of function is precipitated by an unnatural loss of estradiol.
Ovary Removal is Common with Hysterectomy – Now What?
For the millions of women who have had their ovaries removed with hysterectomy, this presents a problem. Amid the myriad of other side effects associated with ovary removal, and perhaps, the root cause of these effects, we can add mitochondrial damage and brain mitochondrial damage, specifically. The rapid decline of estradiol, and other hormones, places many women at risk for neurodegenerative disorders like Alzheimer’s. How could this be mitigated?
In animal research, hormone replacement with 17B – estradiol immediately after the ovaries are removed seems to temper the damage, at least in the short term. There are no long-term studies. Similarly, epidemiological studies in human women suggest hormone replacement immediately after open menopause and/or hysterectomy with oophorectomy reduces clinical symptoms associated with the diseases of aging – e.g. the cognitive decline of Alzheimer’s and other dementias. However, since the synthetic estrogens used pharmacologically are different compounds than those produced endogenously (and used in basic and animal research) and because there are no mitochondrial imaging or even mitochondrial function tests done with human females given hormone replacement, it is difficult to compare the two sets of literature.
Some data suggest that the use of synthetic estrogens damages mitochondria and further diminishes the synthesis of remaining endogenous estrogens (the adrenals continue to produce estradiol and other estrogens after the ovaries are removed). Women who have used synthetic estrogens such as those in oral contraceptives and hormone replacement therapies have lower concentrations of endogenous estradiol, estrone, androstenedione, testosterone, and sex hormone-binding globulin. Based upon the aforementioned research, the decline in endogenous hormones would suggest a commensurate derangement in mitochondrial structure and function, but there are no data either way. At the very least, caution is warranted when contemplating the use of synthetic estrogens, particularly in the current environment that is rife with estrogenic chemicals. There are no data on the use of ‘natural’ or ‘bioidentical’ hormones and human mitochondrial function. So, although the animal data are fairly clear, estradiol replacement begun early enough appears to offset the decline in endogenous estradiol, how this translates to human females is not known.
Other Hormones and Additional Pathways
A flaw common to most research in this field is the failure to address the other hormones involved in modulating health. Estradiol is but one of many estrogens produced endogenously. It is also one of many steroid hormones produced in the ovaries and regulated by mitochondrial function. How estradiol removal or add-back affects progesterone, the androgens, or even the glucocorticoids (cortisol) – is not known. Compensatory reactions are likely. Understanding how those reactions mediate mitochondrial function might determine a viable workaround for the depleted estradiol. The beauty of human physiology is a mind-blowing breadth and depth of compensatory reactions to maximize survival. So I would think, and this is purely speculative, that even if one has lost her ovaries, and even if estradiol treatment was not initiated immediately, or if synthetic estrogens were used instead, there should be other mechanisms to tap into and compensate for this loss. That is, there should be multiple pathways to help maintain mitochondrial function. What those are, I do not know, but they are worth exploring.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image created using Canva AI.
This post was published originally in January 2015.















According to this article https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3702015/ that looked at two cohort studies (one from the Mayo Clinic and one from Denmark), hysterectomy alone (with ovarian conservation), is also associated with an increased risk of dementia. Figure 2 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3702015/figure/F2/ shows the relative risks of “dementia associated with hysterectomy, unilateral oophorectomy, and bilateral oophorectomy stratified by age at the time of surgery in the Danish nationwide study (top block; squares and solid lines) and in the MCSO (middle and lower blocks; circles and dotted lines).”
17-B estradiol is the exact same molecule whether it’s produced in our body or produced by a pharmaceutical corporation. To say otherwise is misinformation. While you didn’t say those exact words in paragraph 11 the idea that 17B estradiol is different when it is produced in or out of our body can be derived from what you said. Perhaps what you meant more exactly is that all animal testing of estrogen effects have not been done with 17-B estradiol ?
Nothing produced at a pharmaceutical company is the same as bodily production.
You don’t have to remove the ovaries to cause the cessation of hormone production. I had a tubal ligation at 28; the aftereffects were the same as if the ovaries had been remove. The ovary is able to discern if there’s a healthy uterus that would need progesterone to facilitate a pregnancy. It’s never a good idea to initiate a pregnancy with a wounded uterus. This is how IUDs work. If you cut the Fallopian tubes, the message to the ovaries is that the uterus is not available for impregnation. This causes progesterone production to fail and estrogen to become dominant which causes all kinds of problems from the resulting inflammation. Unopposed estrogen causes spontaneous abortion. It also causes monthly massive hemorrhaging instead of a normal menses.
It is very important to put progesterone into the equation when trying to understand women’s hormones. Progesterone is the pro-gestational hormone, not estrogen. Menopause is caused by the cessation of progesterone, not the cessation of estrogen. Estrogen is inflammatory; progesterone is anti-inflammatory. After age 50-60, many men have more estrogen than women do; men don’t have ovaries which proves ovaries aren’t required for estrogen production. Estrogen in men causes health problems because it is inflammatory. In women, estrogen dominance, caused by a dearth of progesterone, causes all the damage you would expect to see from runaway inflammation, including cancer.
Progesterone (bio-identical) is an orphan hormone because it cannot be patented. Estrogens, on the other hand, can be created in the lab in all sorts of novel configurations. The world is awash with estrogenic pollution. Soot from a candle provides multiple estrogens from which to choose. The pharmaceutical industry has come up with synthetic “progestins” they tout as being “just like progesterone”. They aren’t. They have estrogenic qualities. Progesterone is a simple molecule; in order to work it has to maintain the exact same molecular structure that is found in nature; you cannot patent a naturally occurring substance. If you can’t patent it you can’t make money with it. So the pharmaceutical industry and the medical industrial complex promote estrogen, crediting their concoctions with all kinds of fabulous attributes. All this promotional hokum has polluted the research because the pharmaceutical industry is ordering what they want proven and paying the tab. Independent laboratory science for the sake of science is pretty much extinct.
I’ve been supplementing with bio-identical progesterone for over 6 years. It has given me my life back. It is available over the counter, no prescription required.
“Sixty years ago, progesterone was found to be the main hormone produced by the ovaries. Since it was necessary for fertility and for maintaining a healthy pregnancy, it was called the “pro-gestational hormone,” and its name sometimes leads people to think that it isn’t needed when you don’t want to get pregnant. In fact, it is the most protective hormone the body produces, and the large amounts that are produced during pregnancy result from the developing baby’s need for protection from the stressful environment. Normally, the brain contains a very high concentration of progesterone, reflecting its protective function for that most important organ. The thymus gland, the key organ of our immune system, is also profoundly dependent of progesterone.
In experiments, progesterone was found to be the basic hormone of adaptation and of resistance to stress. The adrenal glands use it to produce their antistress hormones, and when there is enough progesterone, they don’t have to produce the potentially harmful cortisol. In a progesterone deficiency, we produce too much cortisol, and excessive cortisol causes osteoporosis, aging of the skin, damage to brain cells, and the accumulation of fat, especially on the back and abdomen.
Experiments have shown that progesterone relieves anxiety, improves memory, protects brain cells, and even prevents epileptic seizures. It promotes respiration, and has been used to correct emphysema. In the circulatory system, it prevents bulging veins by increasing the tone of blood vessels, and improves the efficiency of the heart. It reverses many of the signs of aging in the skin, and promotes healthy bone growth. It can relieve many types of arthritis, and helps a variety of immunological problems.”
excerpt above is from here: http://raypeat.com/articles/articles/progesterone-summaries.shtml
Additional well researched articles with extensive references about hormones are available on Ray Peat’s website for free: http://www.raypeat.com/
Very interesting comment! Outside of using progesterone cream which I fear because of quality concerns, are there progesterone rich foods you would recommend? Or is this enough?
Prometrium or it’s generic is an identical molecule to the progesterone that our body makes. It is FDA approved and regulated as to quality and dosage.
If you are using wild yam creams or synthetic progestin (different molecule than progesterone) then you have reason to be concerned. The “all natural” creams not tightly dose or quality controlled.
You will never be able to eat an amount of food to provide you with enough progesterone to keep your uterus lining from thickening and therefor putting you at risk for uterine cance while using estradiol.
Just get Prometrium or generic Prometrium. It is the body identical molecule progesterone. You can order it from some online pharmacies. No there is no food and it’s good that you avoid those creams because dosage and quality is not controlled. You could just brave up and prep ears to see a few doctors and go through the horrible eye rolling and looking at you like you are crazy the way doctors do. It’d be best to have it prescribed by an agreeable doctor even if it takes considerable hardship to find one.
Hi! This is my first time coming across this website researching the pros and cons of hysterectomy. I am 32, have had 3 c-sections and had my tubes cauterized and tied(2014).
I have had debilitating bleeding(golfball sized & larger) clots every period since my last child as well as constant cramping(stabbing pain in my stomach, aching lower back & thighs) that doesn’t subside with ibuprofen. I wear period panties as well as extra large winged pads that I change every hour-hour 1/2 and still bleed through on to my pants multiple times each period.
I had an MRI done on my pelvis 3 years ago for an issue with my urethra and at that time it was discovered that I have adenomyosis.
I have taken hormonal birth control in the past and it made me absolutely nuts. I suffer from extreme fatigue and have gone to the ob multiple times just for them to attempt to continue to shove birth control down my throat which I refuse every time. (I haven’t been back to ob since the urologist discovered the adenomyosis, so that would be new to them if I follow up.)
I recently went in for a physical and had them conduct blood tests and they discovered that my iron levels are extremely low(as well as vitamin D) and I’ve been taking supplements now for 3 weeks and was still low on my follow up blood work. (Both draws were taken between my cycle) and my doctor even commented, “If your levels are this low not on your period, I would hate to see how low they drop when you are.)
I know it’s a lot to read but I’m just looking for guidance. I don’t want to alter my God-given organs, but I also can’t take the pain and fatigue anymore. It literally puts my life to a halt the first 3 days of my cycle every month. Everything I’ve read of adenomyosis says that hysterectomy is the only option. And I’m concerned with the blood loss. I literally feel drugged at the beginning of each period with my energy levels.
Any advice would be greatly appreciated.
Omg this was my life! I as dealing with the exact same symptoms from adenomyosis. It was horrific! I’m 35 and dealt with pain and awful bleeding due 3 years! My dr just kept blowing me off until I almost ended up in the ER for my insane bleeding and clots. I had a hysterectomy because I had tried everything else and nothing helped. The bleeding and pain were getting worse! As soon as I has my hysterectomy (both ovaries intact) I felt a million times better. That soul sucking fatigue was gone along with the pain and constant bleeding. However, I’m about 3 months post surgery and I can tell my hormones are out of whack. I think I’m estrogen dominate and need to take progesterone. I’m supposed to go get blood drawn to see my hormone levels. I know my body and something is off. I need help!
Granted, for the women who have been castrated or whose ovaries have failed after hysterectomy (or via some other means), it is important to attempt to mimic endogenous hormone production. However, the body is too complex to completely compensate for what was lost. In the U.S., there is not even an FDA approved testosterone for women even though according to this study http://journals.lww.com/obgynsurvey/Abstract/2000/07000/Hysterectomy,_Oophorectomy,_and_Endogenous_Sex.20.aspx “Testosterone levels increased with advancing age in intact women and reached premenopausal levels at age 70 to 79 years.”
But the bigger question is “Why are there still so many unnecessary removals of ovaries (and uteri for that matter)?” Studies clearly show that hysterectomy and/or oophorectomy (castration) for benign conditions does more harm than good.
They get paid to do it. It’s a business.
Per Catherine Austin Fitts, the reason why Social Security is going bankrupt is that people are living too long. From the government’s perspective, the solution is to reduce the average life expectancy. Neutering people also helps with overpopulation and Global Warming.