Little known fact. Your reproductive hormones influence how your body responds to insulin. The artificial hormones in hormonal birth control also play a huge role in how your body responds to insulin. And, your body’s response to insulin determines how well you are able to use glucose to supply your daily energy needs.
In this article, we will discuss the basics of how your body creates energy. In this first section, we will unpack:
- How your body creates energy from glucose
- Glucose vs. fatty acids as an energy source
- How insulin resistance impacts the shift between glucose burning and fat burning
- How glucose enters your cells to become fuel for energy
- How insulin resistance interferes with the transfer of glucose into your cells
Then, we will tie in how your natural reproductive hormones, estradiol and progesterone, impact your body’s use of glucose as a fuel source and discuss how hormonal birth control disrupts this natural balance.
How the Body Creates Energy From Glucose
Many of your cell types are designed to run on glucose, a metabolic product of carbohydrates, as their main source of energy, and in fact, certain cells that don’t contain mitochondria (or contain very few mitochondria) like red blood cells and cells of certain parts of your eye (lens, retina, and cornea) rely either exclusively (as is the case for red blood cells) or primarily on glucose as an energy source.
The reason for this is that mitochondria are responsible for aerobic (oxygen required) energy creation processes within your body, and cells with no or very few mitochondria rely mostly on anaerobic (no oxygen required) energy creation by glycolysis in the cytoplasm of the cell. As we will discuss in more detail later, when your body uses fatty acids as a fuel source, this pathway is purely aerobic, so it is not possible for fatty acids to be used in anaerobic energy creation processes within your cells.
When you eat a meal containing sugar (sucrose) or carbohydrates, enzymatic processes begin breaking the sugar and carbs down into their basic structures within your digestive tract. The structure of both sugar and carbs contain glucose.
Glucose fuels the creation of ATP in a process known as glycolysis, which happens within the cell, and through oxidative phosphorylation (OXPHOS), which happens within the mitochondria (substructures within the cell). When ATP is broken down within your cells, it releases energy, which is harnessed to power your mitochondria and other important cellular functions. The by-products of that ATP creation (pyruvate and ATP) fuel additional energy production cascades within the cell.
How the Body Switches From Glucose to Fatty Acids for Energy
Even when particular cell types prefer carbs (glucose) as their energy source rather than fatty acids, most cell types are capable of using either of these macronutrients (and also, when necessary, amino acids) as a fuel in order to survive periods of fasting (including overnight fasting).
Insulin plays a key role in regulating whether your body uses glucose (glycolysis in the cell’s cytoplasm and OXPHOS in the mitochondria) or fatty acids (lipolysis in the cell’s cytoplasm and fatty acid oxidation in the mitochondria) as its preferred fuel source. This is because insulin impacts the ratio of two key enzymes (malonyl Coenzyme A and acetyl CoenzymeA) that determine which of these energy pathways is preferred (here and here). The ratio of these enzymes is dynamic, changing throughout the day in response to when and what you eat, and in response to this fluctuating ratio, your body preferentially uses carbs (glucose) or fatty acids as its fuel source.
In an insulin resistant state, your body does not easily shift between glycolysis/OXPHOS (glucose as fuel) and lipolysis/fatty acid oxidation (fatty acids as fuel) and instead remains in a state of using fatty acids as fuel. We will talk about why this is the case in the next section.
How Glucose Gets Inside Cells
The glucose released in your digestive tract from the food you eat is absorbed into your bloodstream, and when your blood glucose levels start to rise following a meal (or any drink containing carbs or sugar), it signals your pancreas to release insulin.
Insulin is the messenger that lets your cells (specifically, your skeletal muscle, fat, kidney, and liver cells) know there is glucose available in your bloodstream. Insulin does this by binding to the cellular membrane, and this activates glucose transporters on the cellular membrane.
Once blood glucose levels start to drop, a healthy body clears insulin fairly quickly so that it can maintain adequate blood sugar levels. Insulin must be cleared so that blood sugar doesn’t drop too low.
What Is Insulin Resistance?
A number of factors influence how your cells respond to insulin. External influences (like stress, diet, and lack of sleep) along with internal factors (hormonal fluctuations) play a role in how the cells respond to insulin. And, different types of cells respond differently to insulin. Skeletal muscle cells are the most sensitive to insulin. Fat cells and liver cells are also sensitive to insulin, and so these cell types (skeletal muscle, fat, and liver) are the quickest to take up extra glucose from the bloodstream.
When your body becomes more insulin resistant, the cells are not as able to respond to insulin. My favorite analogy for this is to imagine that you are at a rock concert. You cannot easily hear the person next to you because the volume in the venue is so loud that your ears are overloaded by the background noise. In order to carry on a conversation, you must move to a quieter place. In this scenario, insulin is the background noise or the decibel level. When you are insulin resistant, your pancreas releases extra insulin to try to get your body’s cells to respond. This would be the same as somebody yelling at you in a concert hall so that you are able to hear them speak.
When you restore insulin sensitivity, it is like taking your body out of that loud concert hall and placing it somewhere quiet. Now, you are able to hear and carry on a conversation without any problems. When you restore insulin sensitivity, the cells are capable of responding to a much lower amount of insulin much more quickly and take the action of absorbing glucose from the bloodstream.
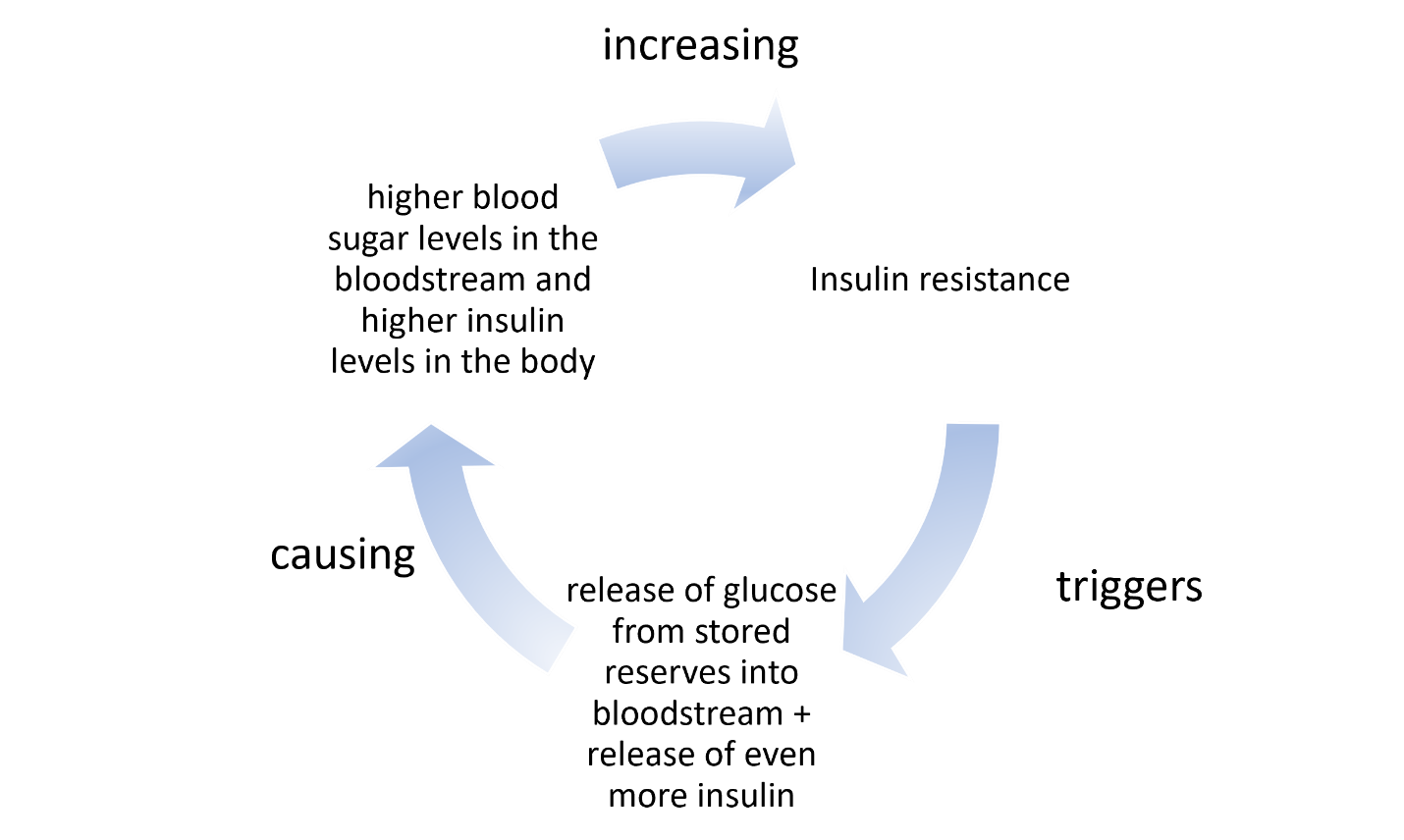
Insulin Resistance Begets Insulin Resistance
With insulin resistance, the cells are used to the high insulin environment (partially deaf to insulin), so they stop responding to insulin’s call. This prompts the pancreas to release more insulin in order to get your cells to hear the message to soak up the extra glucose circulating in the bloodstream. When insulin is unable to be heard because of the high background noise (because there is so much circulating insulin the cells are deaf to it), then glucose isn’t taken up by the cells. This then creates the false message from your cells to key organs to start releasing stored glucose (in a process called gluconeogenesis) to supply the body’s energy needs.
When we are talking about diabetes, this feedback loop often, but not in everyone with diabetes, results in a perfect storm of upward spiraling blood sugar levels.
Even in conditions besides diabetes where blood sugar levels are dysregulated, you might have one condition (for example, insulin resistance), without the other (increased release of glucose from your body’s reserves).
With all of that in mind, let us take a look at how reproductive hormones impact insulin resistance and gluconeogenesis, the process of releasing glucose from stored reserves.
Estradiol, Synthetic Estrogens, and Insulin Resistance
Reproductive hormones play a key role in insulin resistance. Most scientific studies agree that estradiol (the endogenous estrogen produced primarily in the ovaries throughout the reproductive years) boosts the release of insulin from the pancreas. While at first glance, this looks like estradiol might contribute to insulin resistance because it prompts release of extra insulin, the opposite is actually true.
Estradiol is widely accepted as a potent compound to restore insulin sensitivity. Whether this is because of upregulation of insulin from the pancreas or whether it is also because of the influence estrogen has on the cells when it binds to estrogen receptors or a combination of both of these is not clear. What is clear, is that estradiol encourages cellular uptake of glucose and more rapid reduction of blood glucose levels after a meal. Estradiol also reduces gluconeogenesis in the liver suppressing the release of free glucose into the bloodstream from the body’s reserves, and this supports healthy blood sugar levels (here and here).
Estrogen Concentrations and Insulin Resistance
How estradiol affects insulin resistance is concentration dependent. Estradiol concentrations in the bloodstream within the normal circulating range (not more than 1 nanomolar abbreviated 1 nM) are associated with healthy insulin sensitivity and healthy blood sugar levels while concentrations higher than 1 nM are associated with insulin resistance. This may be why gestational diabetes is a common condition during pregnancy with up to 10% of pregnant women in America developing gestational diabetes. Progesterone also plays a key role in gestational diabetes as we will discuss in more detail below.
Non-bioidentical Estrogen and Insulin resistance
Ethinyl estradiol, the most common synthetic estrogen used in hormonal contraceptives here in America, also impacts insulin resistance, but like endogenous estradiol, the relationship is not straightforward. Ethinyl estradiol has been shown to impact insulin sensitivity and gluconeogenesis differently depending on:
- its concentration in the hormonal birth control
- what progestin (synthetic progesterone) it is paired with
Just as high concentrations of endogenous estradiol increase the chances of dysregulated blood glucose control, the synthetic estrogen, ethinyl estradiol, also increases chances of dysregulated blood glucose control. Chemical diabetes caused by hormonal birth control is also well documented in the literature. This is one of the reasons why, since the 1960s, the concentration of artificial estrogens in combined oral contraceptives has been dramatically reduced from upwards of 60 micrograms per pill to as low as 10 micrograms. Currently, most birth control options contain from 20 to 35 micrograms of ethinyl estradiol per pill.
Estrogen Binds to Insulin Receptors Affecting Insulin Resistance
Estrogens, whether synthetic or endogenous, affect blood sugar regulation differently at different concentrations because of their ability to bind to insulin receptors. This concentration-dependent effect of both endogenous estradiol and synthetic estrogens is often overlooked in the conversation regarding the impact of hormonal contraceptives on blood sugar control. Inasmuch as estrogens play a role in insulin sensitivity, insulin secretion, and in gluconeogenesis, and because estrogens are combined in hormonal contraceptives with a wide range of synthetic progestins, the effects on blood sugar regulation are quickly compounded and convoluted.
Progesterone, Progestins, and Insulin Resistance
As with estradiol, the concentration of progesterone also impacts whether progesterone improves or diminishes insulin sensitivity. It is generally accepted that higher concentrations of progesterone during pregnancy are a major contributor to gestational diabetes. Similarly, high concentrations of progesterone, even after menopause, are linked to an increased risk of developing type 2 diabetes.
The actions of progesterone on glucose metabolism is very much related to carrying a pregnancy to term, promoting glucose storage (rather than consumption of glucose for fuel) and promoting ketogenesis (fat burning) within the body. Even when not pregnant, progesterone is the dominant hormone during the luteal phase (second half of your cycle), and this effects how your body uses glucose and its sensitivity to insulin. This ties into common experiences during the second half of your cycle including carb cravings, potentially diminished appetite (if you are like me), and also weight gain.
Unlike artificial estrogens, of which there is only one used in the combined hormonal contraceptives available in the United States, for progestins, the synthetic forms of progesterone, there are four generations of progestins, with each generation containing progestins of different molecular structures. The class of molecules used in synthetic progestins are similar in structure to the endogenous progesterone molecule, but they are not the same. In other words, they are non-bioidentical.
Progestins bind differently to the progesterone receptors within the body (and also bind to a variety of other receptors), than the endogenous progesterone and their specific structure contributes to how much and whether insulin resistance increases. The molecular structure also affects how the body conserves glucose (increases glucose storage) or uses glucose (in the process of gluconeogenesis). It is generally believed that the androgenic nature of progestins determine their role in reducing insulin sensitivity (here and here).
Hormones and Body Composition
An interesting note, whether we are talking about natural reproductive hormones, estradiol and progesterone, or artificial hormones, ethinyl estradiol and the various progestins, these are all fat-soluble hormones. That means, these hormones may be stored in, and thus, impact the behavior of fat cells. One study evaluated the response of fat cells (adipocytes) in the presence or absence of treatment with artificial hormones and found that in the presence of artificial hormones, the adipocytes were more insulin resistant. This suggests that fat cells may serve as a reservoir for artificial hormones and endogenous hormones alike. They essentially soak up circulating hormones from the bloodstream, and these absorbed hormones in turn impact how the fat cells behave.
This finding means that body composition affects how you respond to hormones, whether endogenous or synthetic, and vice versa. It also suggests that, among other things, we ought to consider dosing hormonal contraceptives relative to body composition. Women with higher body fat may store more of the hormones than those with lower body fat and this may initiate or exacerbate insulin resistance.
Summary
In summary, reproductive hormones are intricately intertwined with metabolism, both with how the body creates energy and how it stores fats and carbs to meet energy demands between meals. Hormonal birth control impacts this finely choreographed dance between reproductive hormones and insulin sensitivity, and this seemingly small influence has a dramatic ripple effect. Insulin sensitivity dictates things like weight gain, oxidative stress, and even, as we will discuss in the next article, susceptibility to UTIs and UTI like symptoms.
Before you go, is there someone you know who needs to hear this message? Share this post with them.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.













