With the nutrition wars going on (explained well here), recommending the key macronutrients and their proper proportions for our health, the two dominant camps that have emerged are the carbohydrate proponents and those that oppose the consumption of carbohydrates—some oppose only in “excess” (low carbs, ketogenic, Atkins, etc.,) and others “completely” (zero carbs). Between the members of these groups, angry words are exchanged, and competencies, educations, and other personal nonscientific arguments are bandied around. I call this nutrition bullying. And then there are the substantive conflicts and inconsistencies. Like the following confusing statements – 10 pages apart in the National Academies of Sciences Dietary Reference Intake (DRI) guideline book.
In the chapter titled Clinical Effects of Inadequate Intake on page 265 the opening statement is as follows:
“The Recommended Dietary Allowance (RDA) for carbohydrate is set at 130 g/d for adults and children based on the average minimum amount of glucose utilized by the brain.”
Going to page 275 in the same chapter, we read:
“The lower limit of dietary carbohydrate compatible with life apparently is zero, provided that adequate amount of protein and fat are consumed”.
As you can see: on the one hand, dietary carbohydrate is needed for the brain, and on the other hand, the carbohydrate need is zero for life (thus, zero for the brain). If we had a third hand, I would like to hold in it the USDA recommendations passed on to all nutritionists, suggesting that the ideal carbohydrate intake is 45-65% of the daily Calories. For a typical 2000 Calorie diet (as it is on all food labels) this comes to 225 – 325 gr carbohydrates a day. Thus, we are told that the human body needs zero carbohydrates to stay alive, provided that fats and proteins are consumed in adequate amounts, and also that the RDA is 130 gr carbohydrates for the use of the brain that needs no carbohydrates, while the USDA recommends 225 – 325 gr carbohydrates. Major confusion! Even worse, this confusion is not well known; it goes unnoticed by almost all scientists, dietitians, and nutritionists—not to mention the general public. I would like to shed some light to the sources of this confusion, hopefully providing you with much needed clarity on this hot subject.
Let the Carbohydate War Commence
From an academic perspective the war makes a lot of sense. After all, those who have supported the high carbohydrate paradigm of the Standard American Diet (SAD) have built their careers on its credibility. Whether they themselves follow the recommendations of the SAD or not, they have a vested interest in maintaining their stand in the high carbohydrate field. Similarly, those whose lifelong research has been in the low or zero carbohydrate fields have a vested interest in sticking to their guns.
Those not members of either camp (many scientists, nutritionists, and almost all people in general) can be forgiven for feeling like spectators on the sidelines of a tennis match, during which one’s head ends up spinning from looking left and right nonstop. Many people decide to just jump head first in and test the waters to see where they end up. This causes a lot of problems because macronutrients represent life sustainment and are not up for games and self-experimentation—people can get hurt. Each macronutrient has its very specific quality. Some are necessary for the body to keep it healthy and others are not needed at all or can even be harmful. An educated choice is a better approach but beyond the above described controversy, there is much misinformation on the internet, creating further confusion.
Macronutrient Choices: What They Do and Do Not Do
There are three macronutrients: carbohydrates, proteins, and fats.
Carbohydrates
Carbohydrates are all plant matter: all fruits, vegetables, nuts, seeds, and grains. While many people think that vegetables, fruits, and whole grains are “not carbohydrates”, only sugar and desserts are “carbs”, in reality, all carbohydrates turn into sugar in our bodies. In this sense, there is very little difference between eating 4 grams of sugar from a teaspoon or 4 grs sugar equivalent from an apple or a slice of bread.
Carbohydrates can be “free glucose”, such as the teaspoon of glucose or the amount of glucose in a fruit, or they can be attached to fiber and need separation, or to other carbohydrate forms that need to convert to glucose, such as fructose, starches, galactose, or lactose. Those carbohydrates that need any type of conversion by the body into glucose are not listed as “sugar” on product labels. In general, on every food label you find sugar (free glucose), fiber, and carbohydrates. Since fibers don’t convert to sugar, to find out the total amount of sugar that will become active sugar in the body, we need to subtract fiber from total carbohydrates.
Here is an example to help you understand what I mean: take a slice of unsweetened whole wheat bread from the USDA database. You will see the following on the label and in [] are my explanations:
Carbohydrates by difference: 12.11 gr [total carbohydrates]
Fiber: 1.7 gr [both soluble and insoluble]
Sugar, total: 1.23 gr [free sugar].
We know that a slice of unsweetened wheat bread like this doesn’t taste sweet, yet, if you subtract the fiber from the total carbohydrates, the actual sugar amount in the slice of whole wheat bread is 12.11 – 1.7 = 10.41 gr. This amount truly represents everything that is either glucose or that converts to glucose in the body and not only the sweetness value the slice of bread has by its free sugar content. The actual sugar amount for the bread is 10.41 gr, or almost 3 teaspoons of sugar, in a food item that nobody considers sweet.
Every single carbohydrate item you can think of provides mostly sugar to the body in terms of macronutrients—very little protein and fat. Carbohydrates can also provide micronutrients, such as vitamins, minerals, and various antioxidants, plus fiber. However, we must remember that, according to one of the above quotes, supported by the real-life experiences of many ethnic/tribal societies and those individuals who have followed a carb free diet, carbohydrates are not essential for life at all. We can completely live a healthy life without a single slice of bread, without a single apple, or any other carbohydrates. How about the micronutrients in carbs and fiber: do we need those? The answer must be “no” if we have zero need for carbohydrates—therefore, carbohydrates are not an essential macronutrient.
Proteins
Proteins are mostly in animals and seafood. I created a table listing all amino acids—proteins are made from amino acids.
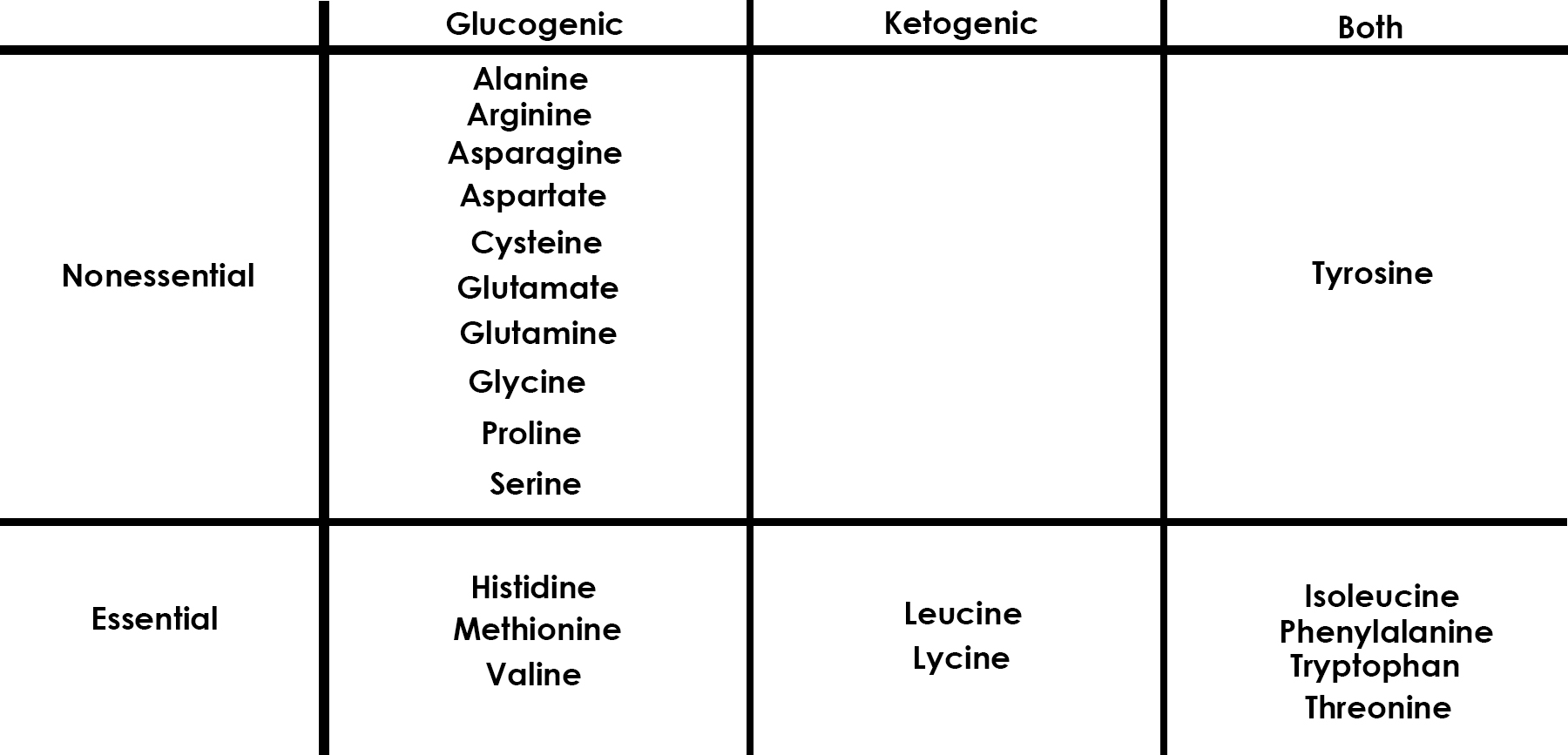
We have two types of amino acids: essential and non-essential. Within the non-essentials, most are glucogenic (meaning they convert to glucose), and one can be converted either to glucose or to ketones. Among the essential amino acids, three can only convert to glucose, two only to ketones, and four to either. Two questions should pop into your mind immediately: 1) Is there a reason why some of the amino acids convert to glucose and others to ketones and 2) why do we have amino acids that only convert to ketones? The answer is quite simple: the body can use two fuels for energy: glucose and ketones and it needs to have the ability to move between these two metabolic processes seamlessly. Thus, amino acids that can only be used as ketones, can be used by our body very well. The reason for some to only convert to ketones is that some cells in the body (including the brain that controls Parkinson’s disease1 and Alzheimer’s disease) work better and improve while using ketones.
Lastly, plants contain little protein compared to animal/seafood sources, therefore, those with a mostly vegetarian or vegan diet are greatly disadvantaged in the essential amino acid category.
Fats
The third macronutrient class is fats (fatty acids). Fatty acids are found is all animal sourced foods, including seafood and, in some carbohydrates—not all. Unlike carbs or proteins, all fats are essential. We typically discuss fats as saturated, monounsaturated, and polyunsaturated fats, but in reality, these three fat types are always found together in nature, so it is best to discuss fats from the perspective of what type of omega fats they are. There are several but the most well-known are omega 6 and 3. Omega 6 can be found mostly in plant-based foods and some in animal fatty acids, and omega 3 is in mostly animal/seafood sourced foods. There are three types of omega 3 fatty acids: ALA (from plants only), EPA and DHA (from animal and seafood only). The human brain is over 60% fat, much of it is DHA (EPA is a precursor to DHA) and since that is only found in animal/seafood sources, eating meats and seafood is essential. Those who get their omega 3s as ALA from carbs are in trouble, because the human body is not capable for quantity conversion of ALA to EPA or DHA. This causes some major problems for vegetarians and vegans—males and females differ slightly in conversion rates2,3.
Are We Eating Foods or Drugs?
You are thinking “how silly is this question? Of course, we are eating foods.” Hold that thought. We need to understand the hormonal connection to be able to answer the question if certain foods can be drugs. If we eat something that is not needed for our life and survival, such as a carbohydrate, what role will it play? There is a battle going on inside your body as you eat; the battle of hormones, how macronutrients affect them, and how your brain reacts to what you eat. This is currently a highly controversial topic between the two warring camps of scientists. I want to present here some of the arguments in this debate.
Let’s talk about hunger and what drives hunger considering the macronutrients we discussed—focusing on carbohydrates, the subject of the most heated debates.
A scientist colleague, Dr. David Pendergrass, describes what food is and what it does in terms of our metabolic and endocrine (hormonal) system very eloquently on his blog:
“Clearly carbohydrates are not drugs in the same way that heroin is. They are indeed nutrients. Yet they activate the dopaminergic mesolimbic pathway (so called rewards or saliency pathway depending upon the neurobiologist you happen to be talking to…), in the same way heroin, nicotine, and alcohol do. To that end…, it has drug-like capacity. The neurobiologist perspective to addiction is that down-regulation of receptors MUST occur and that withdrawal syndromes occur. Heroin and opiates are addictive under that qualification as the opiate receptors downregulate via intracellular Ca++/phosphorylation events, decreased receptor expression and receptor withdrawal mechanisms…So by this definition, carbohydrates may indeed be considered addictive because of the insulin receptor down regulation (AKA insulin resistance) that occurs with chronic hyperinsulinemia. Since insulin is considered an anorexogenic peptide, then you would need progressively more carbohydrate to induce satiety as more and more insulin is needed to bind to insulin receptors to achieve the same results. This particular description might well merit the term addiction in the down-regulation sense.
Addiction by a behavioral definition is different. It suggests that anything drugs (carbs, alcohol, sex, gambling, food) that is patently ‘bad-in-excess’ or to the point that it affects health or work or relationships and is difficult to stop, would be an addiction by psychologists. In these cases, there is neuronal reinforcement of the behavior by the compulsion. This neural plasticity is accompanied by specific changes in neurotransmitter release and receptor organization across the synapse. Indeed, increased numbers of synapses occur with such compulsions. Again, this is a function of the behavior-causing neuronal rewiring in the dopaminergic mesolimbic pathway that supports the compulsion. In this manner and definition, carbohydrates by a psychological definition would also be considered addictive.”
It is important to recognize the differences between – let’s say – opioids and carbs. The process of down-regulation, the reduction in receptors in numbers and sensitivity, takes significantly longer for carbs, allowing for the development of a chronic condition we know as type 2 diabetes, considered to be a terminal chronic disease if left untreated. Actually, type 2 diabetes can be reversed in most cases—this is a subject for another article in the future. Studies show that some foods—those with high glycemic index (GI)—seem to activate those reward pathways in the brain that are also activated by street drugs. Furthermore, ghrelin, a hormone involved with hunger and satiety is also involved with the reward brain circuit in both food and drug-induced reward mechanisms.
In any case, both with street drugs and carbs, the receiving hormone or neurotransmitter (in the brain) loses its receptors or their sensitivity to deliver the drug or carbs to the target cells4. With such identical mechanisms and ultimate consequences, eating carbohydrates suspiciously looks like an addiction. Furthermore, we must ask what makes quitting carbohydrates so difficult. Many people struggle to quit—often quitting for some time and then returning, unable to hold sweet-free life. This table, “relative sweetness value”, shows some really scary numbers. Natural sugars, such as sucrose and fructose, are significantly sweeter than glucose by taste—is sweetness the driving factor? Apparently, it may just be so5. It is worthy to note that while fructose is the sweetest of all natural sugars at 110 in relative sweetness factor, glucose is only 74, so there is a significant difference between them—compare this to lactose in milk at 16. Aspartame, a very common sugar substitute has a relative sweetness factor of 18,000! Wow! If relative sweetness value alone drove sugar addiction, then sugar substitutes would elicit an addiction as well—and indeed they do. “Intense Sweetness Surpasses Cocaine Reward.” And while my initial hunch was that since fructose has a higher relative sweetness value than glucose, it would elicit a higher reaction in terms of addiction, this is not the case. A specific scale, the Yale Food Addiction Scale (YFAS) was developed to assess food addiction.
From an evolutionary standpoint, getting addicted to something is not a good thing as withdrawal (withdrawal is a necessary component of addiction) produces weakness and works against the survival of the fittest. In the long history of human evolution, glucose/fructose were not available in big quantities, and so addiction danger was never present. This also immediately implies that because of the short/seasonal availability of glucose and fructose, it would have created an evolutionary advantage to those whose carbs cravings was strong and could gobble up all that was available when it was available. Therefore, what we now label as addiction, at one time may have had a different role and vastly different manifestation—without withdrawal—serving as a benefit to human kind. Research also found that reactive hypoglycemia (RH), a form of insulin resistance where glucose levels drop drastically after eating, initiate a different brain response from those subjects without RH. RH subjects seek higher carbohydrate and caloric content foods. In addition, there are “brakes” in the intestines and the gut area of human. Such brakes serve to cause satiety or hunger, which is based on factors of BMI, age, and gender.
Only in the very recent past have been high glucose/fructose containing foods and drinks readily available. Over-consumption of highly sweet carbohydrates don’t activate our satiety hormone (ghrelin) the same way as protein or fat does. “[G]hrelin activates an important reward circuit involved in natural- as well as drug-induced reward, the cholinergic-dopaminergic reward link”. It also appears that co-factors are involved: people with higher level of alcohol consumption may crave more sweets and those with higher consumption of sweets may crave more alcohol.
There is much more research needed to understand the exact mechanism of sugar and sweet carbohydrates cravings, though it seems clear that highly processed, fast-absorbing carbohydrates share pharmacokinetic properties with drugs of abuse. While sugar or processed carbohydrates are not likely to be classified as drugs in the near future, further evaluation for what they do to the human body is warranted, particularly given the obesity and metabolic syndrome crisis we are facing. As stated all through, carbohydrates—including both highly processed and non-processed types—are not essential for us to eat.
The biggest question we need to ask is how can something that takes up such a large percent of our caloric intake – and does so unnecessarily – be ever eliminated from our diets. Should carbohydrates be regulated by taxation and advertisement controls similarly to tobacco and alcohol? Or are we ready to continue long-term chronic disease treatments at astronomical costs because eating carbohydrates is so culturally ingrained?
Sources
1 VanItallie, T. B. et al. Treatment of Parkinson disease with diet-induced hyperketonemia: A feasibility study. Neurology 64, 728-730, doi:10.1212/01.Wnl.0000152046.11390.45 (2005).
2 Burdge, G. C., Jones, A. E. & Wootton, S. A. Eicosapentaenoic and docosapentaenoic acids are the principal products of α-linolenic acid metabolism in young men. British Journal of Nutrition 88, 355-363, doi:10.1079/BJN2002662 (2002).
3 Burdge, G. C. & Wootton, S. A. Conversion of α-linolenic acid to eicosapentaenoic, docosapentaenoic and docosahexaenoic acids in young women. British Journal of Nutrition 88, 411-420, doi:10.1079/BJN2002689 (2002).
4 Figlewicz, D. P., Bennett, J. L., Aliakbari, S., Zavosh, A. & Sipols, A. J. Insulin acts at different CNS sites to decrease acute sucrose intake and sucrose self-administration in rats. American Journal of Physiology – Regulatory, Integrative and Comparative Physiology 295, R388-R394, doi:10.1152/ajpregu.90334.2008 (2008).
5 Murray, S. M., Tulloch, A. J., Chen, E. Y. & Avena, N. M. Insights revealed by rodent models of sugar binge eating. CNS Spectrums 20, 530-536, doi:10.1017/S1092852915000656 (2015).
We Need Your Help
Hormones Matter needs funding now. Our research funding was cut recently and because of our commitment to independent health research and journalism, unbiased by commercial interests, we allow minimal advertising on the site. That means all funding must come from you, our readers. Don’t let Hormones Matter die.
Yes, I’d like to support Hormones Matter.
Image by Aline Ponce from Pixabay.















