Recent attention in a dual Reveal and Kaiser Health News Report (‘Kaiser Report’) to the risks of Lupron’s use in children with central precocious puberty (PP) or growth issues, and to Lupron’s risks in general, presents an opportunity to continue the disclosures on the risks of Lupron. This is the fifth part in a 6-part series exploring numerous areas addressing the use of Lupron in the pediatric and teen population. The series began with the voices of the mothers of harmed children and the now-adult suffering children. This was followed by articles on the regulatory issues that surround Lupron’s approval and continued use, the possible reproductive injuries associated with this and other drugs within its class, and issues surrounding Lupron’s metabolism and clearance from the body. Here we will take a look at some of what is known about the Lupron money trail.
Ignoring and Dismissing Side Effects: Follow the Money
WebMD, a highly ranked and promoted consumer ‘go-to’ site for health information, ‘informs’ the public about precocious puberty: “[t]here’s no evidence that these [GnRHa] drugs cause any long-term problems”. Common neurological and musculoskeletal complaints from Lupron, such as joint and muscle pain, and mood changes are listed as “infrequent” and decreased density of bone as a “rare” side effect. WebMDs “Fertility Drugs” page fails to identify Lupron as a ‘Pregnancy Category X’ drug (as designated by FDA), but states “as many as 50% [with successful ovulation] are able to get pregnant. Most side effects are mild.” Another high-ranking consumer information website, Medscape, tells of a number of clinics “all very experienced in treating gender dysphoric youth … This [GnRHa] treatment is fully reversible.” (See ‘Lupron and reproductive injury’.)
While unrelated to Lupron, the following news story from 2009 was nonetheless thought-provoking: Medscape and WebMD were accused in a whistleblower lawsuit (involving 17 states) of being “part of an illegal conspiracy to promote the off-label use of two [drugs]” – and the details of the charges were “a mystery” due to major redactions by the judge.
Lupron is no stranger to whistleblower lawsuits (here , here, and here) or to charges of promoting off-label uses. The drug’s manufacturer has received ‘Notices of Adverse Findings’ due to its promotion (“indoctrination“) of Lupron for unapproved gynecological indications, and warnings for misleading claims in its prostate indication. The company’s schemes of fraudulent drug pricing and bribing doctors are well known and documented.
CafePharma, an anonymous industry insider message board for pharmaceutical sales reps, had a few postings in 2010 that summed the scenario up succinctly.
“[T]he docs know who has buttered their bread, and we [drug company/sales force] got very deep pockets” (see post of March 20, 2010 @ 12:25 pm here). And “YOU DUMMY ABBOTT PAYS MILLIONS UNDER THE TABLE SO DOCS USE LUPRON (emphasis in original)” (see post of March 27, 2010 @ 7:45 pm here).
How Lucrative is Lupron Use in Precocious Puberty?
The Kaiser Report identified that in a 2 year period of time Lupron’s manufacturer, AbbVie, had paid $157,066 to the lead investigator of Lupron’s precocious puberty clinical trials, Dr. Peter Lee (a pediatric endocrinologist). According to ProPublica’s “Dollars for Docs”, for the years 2015, 2014, and 2013, Lee received from AbbVie a total of $102,325 for “Promotional Speaking/Other” for Lupron. (Payments by AbbVie to Lee for Lupron related “Consulting”, “Travel and Lodging” and “Food and Beverage” were not tallied, but figures are available at ‘Dollars for Docs’/ProPublica for each of those 3 years.)
The Kaiser Report also identified that both AbbVie and investigator Lee did not answer specific questions about the omission of serious adverse events (a bone disorder and a pathological fracture) in a key pediatric clinical trial of Lupron. How is this acceptable? If the drug company and lead clinical trial investigator will not answer questions about adverse events in the trial – who will?
In the drug company’s campaign to promote Lupron for precocious puberty (entitled “Too Soon”), they claimed (in 2003) “[t]here are almost 5,200 children who have central precocious puberty and grow up too soon” (see Question/Answer # 10). Lee was a member of the editorial board of “Too Soon”, and Lee is a consultant for AbbVie, and “has received payment for the development of educational materials by AbbVie”.
It goes without saying that during a promotion of something (especially if one is being monetarily compensated for doing so), such promotion usually results in a loyalty to, and liking for, ‘the thing’. And especially so if ‘the thing’ is a “cash cow” (stated in a ‘CafePharma’ post of August 8, 2011 @ 3:47 pm).
In 28 months (August 2013 through December 2015), AbbVie made 69,173 payments related to Lupron for a sum of $16.9 million to 24,910 doctors, and Lee came in second place in ‘top doctors receiving payments related to Lupron’.
How objective can Lee and the other 24,909 who are paid by the drug company to promote Lupron be? What would happen if any one of the 24,910 paid Lupron spokesmouths were to say “Hey, wait just a minute … there’s some pretty sick kids (or men and women) out there after using this drug – we need to take a serious look at this”?
Simple logic should tell you that a pharmaceutical company does not spend $16.9 million over a 28-month period to almost 25,000 doctors to hear a negative (bad) message about its product. In fact, I have seen signed consultant and scientific advisor agreements by a rheumatologist with this drug company, and there was a pledge taken to defend the company’s products at all times in all ways (documents presently unavailable, but reference to them was made in my 2003 congressional testimony, p. 12).
It seems peculiar that the #2 recipient of payments for the promotion of Lupron (the use of which spans multiple adult male and female indications that number in the millions) would involve a specialty that serves not quite 5,200 children.
Lupron’s use in the pediatric population is not limited to precocious puberty, and extends to youths and teens with gender dysphoria. Estimates from a federal database in 2016 place the numbers of adults who identify as transgender at 1.4 million (with states ranging from 0.30% to 0.75% of population), but there are no national surveys of youths; small-scale high school surveys have shown about 1.5% of surveyed students identified as transgender.
Pain and Agony of Adverse Effects Is Not a Lucrative Message
In an “ethical dilemma of choosing [between] wrongly suppressing puberty in kids who will grow out of their gender variance or refusing treatment [Dr.] Peter Lee … who had [by 2007] treated three young transgender teens with Lupron, knows on which side he’d rather err” – and that is to administer Lupron/GnRHas. Dr. Lee described one transgender adolescent 20 years ago “in so much pain and agony” that she later committed suicide. (A different perspective has been offered from a psychiatrist who has called this “Lupron treatment [for transgenders] a modern form of child abuse“.)
Where is the discussion on the pain and agony of pediatric (and adult) Lupron victims, and the psychological and psychosocial effects upon the child after development of medication adverse events? (See Part 1 of this series for excerpts of heart-wrenching pain and agony voiced by parents and victims.) The sudden onset of migraines, weight gain, joint and bone pain, muscular pain, weakness, mobility limitations, mobility impairments, mood changes, irritable bowel, lethargy, difficulties with concentration and memory, anxiety, depression, suicidal ideation, etc., following treatment would indeed have a profound impact upon the child, their relationship to peers, and academic participation.
Given the flood of complaints about Lupron injury that is posted at various online sites, the $64,000 question remains ‘why has the pain and agony experienced by Lupron victims (of all ages and all genders) been so marginalized and often dismissed’? What causes the reported anger and defensiveness doctors have displayed when queried about the medication adverse effects? (See petitions and medication review site links – the web collectively provides millions of posted complaints, with daily additions.)
Marketing Indoctrination and Coercion
In March 1990 the FDA sent Lupron’s manufacturer a ‘Notice of Adverse Findings’, concerning its “deliberate campaign to promote this product for a wide range of unapproved uses.” A follow-up memo further detailed the FDA’s “concerns” about an upcoming drug company sponsored program at “Walt Disney World Swan”: the FDA said “it appears to be a program to indoctrinate physicians in unapproved uses of Lupron, and to specifically encourage administration of Lupron for these unapproved uses.” These unapproved uses involved gynecology and fertility. (In October 1990, Lupron received FDA approval for the indication of pain management in endometriosis; no FDA approval for fertility treatment has ever been obtained – and note that Lupron’s initial patent was for ovulation induction.)
As an IVF patient in 1990, my fertility clinic’s brochure stated “Lupron is only prescribed to persons with certain diagnoses”, but in 1991 this changed to “Lupron is widely prescribed”. What would cause the sudden universal use of Lupron at this (and just about every other) IVF clinic? A 1992 study, which asked in its title whether there was any medical advantage for using GnRHa’s for all patients undergoing IVF, concluded:
“The routine use of GnRH-a for all patients undergoing IVF has practical but no significant medical advantages … there have been very few prospective randomized studies comparing the use of GnRH-a with conventional stimulation regimens”.
My IVF clinic’s doctors had become indoctrinated to use Lupron in ovulation induction in the same manner as IVF clinics throughout the country. A 1989 US Subcommittee mailed a detailed survey to 224 US fertility clinics to obtain a wide variety of IVF data, and in the process many clinics self-reported their new ‘Lupron protocol’. These survey responses, and transcripts of an accompanying hearing, were published in a document titled “Serial No. 101-5” (101st Congress; March 9, 1989). Here are a few pertinent excerpts illustrating the abrupt change to using Lupron by the survey respondents:
“Changing to Lupron stimulation for all patients” (p. 333. ART Program, Birmingham AL), “us[ing] Lupron for all patients” (p.408. Fertility and Reproductive Health Institute of Northern California, San Jose, CA.), “seventy percent of all patients are administered leuprolide” (p. 417. Century City Hospital, Los Angeles, CA.); “in 1988 we initiated the use of GnRH agonist for all patients” (p. 490. Hoag Fertility Services, Newport Beach, CA.).
Of the hundreds of fertility clinics responding to the Subcommittee survey, only one clinic raised a word of caution:
“Promoting the Use of GnRHa (Lupron) … it remains entirely unclear that all patients need this costly and often painful [and “experimental”] approach” (p.852. University of Medicine and Dentistry of New Jersey, Robert Wood Johnson Medical School, New Brunswick, NJ.).
Men, told they otherwise would face treatment for prostate cancer by either castration or DES (and potentially experience gynecomastia and adverse cardiovascular effects) were ‘encouraged’ to use this drug. A survey of urologists revealed that 53% did not believe in the efficacy of GnRHa treatment but still prescribed it.
My 2003 congressional testimony identifies (p. 7) “the badgering, and coercion, and manipulation, and threats used to convince women into taking Lupron for a variety of indications – many refer to their doctor as trying to “shove it down [their] throat”.
Women were threatened with a hysterectomy (endometriosis), the specter of bleeding to death (fibroids), or refusal to undergo IVF. My 1993 testimony to the MA. Health Care Committee (an attempt to enact legislation which would mandate fertility clinics provide, among others, accurate information on the risks of Lupron) states: “… nearly every IVF clinic has mandated that women take Lupron – or they will not be allowed to cycle.”
Parents of children with precocious puberty are ‘encouraged’ to use this drug to prevent the child from ‘enduring psychological distress from their precocious development’ and to ensure achievement of ‘appropriate’ height. In the transgender population, a similar psychological premise is offered for the normal – but ‘unwanted’ – sexual development, and the specter of anxiety, depression and suicide is raised for the untreated dysphoric youth/teen.
History of Fraudulent Data
In a review of the endometriosis clinical trials’ raw data, Dr. David Redwine discovered that the raw data did not support the claims by the company. In one example, Redwine’s analysis revealed that
“62.5% of women had not regained baseline estrogen levels one year after stopping Lupron … This is definitive evidence of long-term damage to ovarian function.”
Yet, contrary to this raw data, Lupron’s endometriosis label states the effects of Lupron “are reversible upon discontinuation”. (See p. 26 in amicus curiae for US Supreme Court.) If 62.5% of subjects one year after Lupron discontinuation evidenced long-term damage to ovarian function, then what data did the company provide to the FDA for its 1990 Lupron approval which ‘demonstrated’ its effects “are reversible upon discontinuation”?
In 2010, Dr. Redwine provided a 300-page report to the FDA concerning these instances of apparent data fabrication. The essence of his report, titled “Leuprolide – the ‘D’ is Silent”, can be seen in a somewhat redacted power point presentation here. Years after receiving the report, the FDA decided “no regulatory action is needed” – all the while ignoring and failing to address the issue of fraudulent data and altered outcomes delineated in this report. ‘Lupron Victims Hub’ sent an Open Letter to FDA in 2014 with specific questions – those questions remain unanswered.
During the lawsuit ‘Klein v. TAP, Abbott’, Redwine served as an expert medical witness, and in his expert statement he describes Lupron’s “medical fraud” as being “the most egregious example of Big Pharma controlling the practice of medicine”. Dr. Redwine concludes that Lupron is “unsafe and harmful in addition to being ineffective”.
For further information on retraction of Lupron studies and other instances of problems with the data in Lupron studies, see here, here , here , here, and here.
Considered Not Related to Study Drug by the Investigator
In the Phase 3 and Phase 4 clinical trials by Dr. Lee for 1 month Lupron Depot-PED, one subject died from respiratory infection and heart arrest. In typical Lupron clinical trials’ language, this adverse event was “considered not related to study drug by the investigator”. Of the 7 subjects for which serious adverse events were reported, 5 of those 7 subject’s adverse events were “considered not related to study drug by the investigator”.
In another precocious puberty study, the only serious adverse event reported was increased intracranial pressure, and this also was “considered not related to treatment by the investigator”. While this subject did have a ventricular-peritoneal shunt, it should be noted that Lupron is known to be a cause of increased intracranial pressure. And so it would be interesting to learn how long – prior to Lupron – this subject had a shunt in place without any increased intracranial pressure. Inclusion criteria for entrance into this study require “general good health with no uncontrolled, clinically significant disease”, and exclusion criteria preventing entrance into this study were “any concomitant medical condition that, in the opinion of the investigator, may expose a subject to an unacceptable level of safety risk”. (And note an unrelated post by a 24 year old woman who developed pseudotumor cerebri “as a result of the poison Lupron”, and who requires a shunt: see July 25, 2011 entry @ 10:38 am here.)
I suppose there could be a number of different reasons for an investigator to consider an adverse event as “unrelated” to a drug, but unless specific questions about the adverse events from these pediatric trials are actually answered — knowing the history of this drug — I can only assume the worst.
Questionable Data Found in Adult Male and Adult Female Studies
MEN: In the mid-1990s, after scouring FDA documents related to Lupron’s initial approval for prostate cancer, it appeared there was curious and questionable data related to Lupron’s cardiovascular effects. At the time, I questioned the validity of the claim Lupron had a safer cardiovascular profile than alternative treatment – a mantra that became a selling point for the drug. (See ‘Was Lupron’s Initial FDA Approval Based Upon Safety & Efficacy’, p. 4-10 here). In 2010 the FDA would issue warnings for Lupron/GnRHa use in men concerning the potential increased risk for cardiovascular problems, heart attack, sudden cardiac death, and stroke (and diabetes).
WOMEN: In my 1995 testimony to the MA. Health Care Committee, I identified “manipulated figures” (p. 8 here) in a female Lupron study – fourteen months before the Federal Register posted a Notice of Scientific Misconduct about the same Lupron investigator/author who had been found guilty of falsifying and fabricating 80% of data in 4 other Lupron studies (2 of which had been published and required retraction).
Illegal Marketing Schemes in Gynecology and Urology
Years ago I was aware of a gynecologist approached by the drug company’s sales force that indicated he could clear $98,000 to his income by prescribing Lupron” (see page 8), and would also find an internal confidential company memo unearthed during Oversight Hearings which detailed for urologists the annual $105,011.40 doctors could earn when they prescribed Lupron.
Bloomberg News summed up the impact drug money had in urology (‘Prostate Patients Suffer as Money Overwhelms Best Therapy’, November 6, 2012. Bloomberg News; article snippet here):
“[In the past] Urologists could make $5,000 per patient dispensing Lupron in their offices, thanks to secret discounts and kickbacks from drug makers. … In 1997 the 25 top-prescribing Lupron urologists each averaged $1.6 million in Medicare payments. … Two of every five patients who received hormone therapy didn’t need it, the [New England Journal of Medicine] study found. In 2005, after Medicare cut Lupron and Zoladex payment rates by over half, inappropriate use plummeted 44 percent. … Hundreds of thousands of men were chemically castrated for no reason; that’s the biggest scandal of all. … The money was too irresistible.”
There were reports of bribes from Lupron’s sales force in both urology and gynecology, and ultimately
“the company pleaded guilty to participating in a criminal conspiracy by providing doctors with free Lupron samples for which doctors then billed Medicare [with] the company inflat[ing] the list price of Lupron to ensure that doctors who prescribed it would make a sizable profit when the government reimbursed them.”
The company paid the then-highest fine in US history – $875 million.
In addition to my multiple attempts to encourage the US investigation to expand its investigation from financial fraud and into the health risks posed by Lupron, it appears others were also making similar requests: “A call to the U.S, Attorneys Office inquiring whether financial fraud in the marketing of Lupron might indicate that FDA studies may also have been fabricated brought no answer. They are simply not interested.”
Paying the Patient Support Groups
In the past, “[i]n addition to offering inducements to hospitals and doctors, [Lupron’s manufacturer] was encouraging its salespeople to approach patients in support groups” (see here, here, and here ). It is known that the manufacturer of this drug and other GnRHas contributed hundreds of thousands of dollars to an endometriosis support association , and Lupron’s manufacturer also contributed thousands and thousands of dollars to a fertility support group (at a time when Lupron was only FDA approved for men). It is only logical to question whether any pediatric support group(s) experience(d) ‘infiltration’ of Lupron money.
One pediatric group dedicated to growth disorders, the Magic Foundation, is known to have received money from growth hormone manufacturers. According to publicly available documents from Guidestar, this foundation has reported 2014 contributions of $949,348 (contributors’ identity not provided). Appearing prominently (and to me, appearing promotionally), the Foundation’s website discusses and displays Lupron Depot-PED information, as well as providing the web address for AbbVie’s Lupron Depot-PED product information. (Until recently, no other GnRHa was identified, discussed, or linked on the Foundation’s website, and presently one other 12-month injectable, non-Lupron, GnRHa drug is mentioned.)
The information posted on the Foundation’s website of risks from Lupron Depot-PED is quite sparse: there is mention of temporary mood changes, injection site redness and pain, and rarely a sterile abscess, concluding “[r]esearch to date indicates that when treatment is stopped, puberty should resume and advance normally.” “Only as a convenience” does an AbbVie “Puberty Too Soon” website provide a web link to the Magic Foundation. It should be noted that AbbVie’s lead Lupron precocious puberty investigator Dr. Peter Lee, is on the Medical Advisory Board of the Magic Foundation.
Transgender Use of Lupron Noted as Lucrative for Some Providers
A 2013 ‘GenderTrender’ article noted for years “a cluster of extremely well-funded physician providers” have been prescribing to children off-label drugs for transgender use. This article states Lupron is “so toxic” adult transgenders are advised against its use. The article includes a statement by Lee: “Suppression … can be effectively and safely accomplished using GnRHa – an intervention that is both temporary and reversible.”
Benefits of Orphan Drug Status
Lupron for use in precocious puberty (a rare ‘orphan’ disease‘ which by definition affects less than 200,000 in the US) has the designation of “Orphan Drug” status, allowing the drug company tax credits (under 26 USC 45C) for related clinical testing expenses (see here and here). It should be determined if expenses from non-precocious puberty pediatric uses (which would be ineligible for orphan status/tax credits) have been filed, i.e., transgender and acne (which affects approximately 1.4 million and 50 million people, respectively). How many off-label, unpublished studies have been conducted in the pediatric and teen population?
Lupron is Lucrative
Based upon the information provided here (and this is not an all-inclusive list), in my opinion it seems little wonder that Lupron became the most prescribed GnRHa, became prescribed for men, women, and children (and animals, fish, chickens, etc.). And it’s no surprise why Lupron has been prescribed for A – Z off-label indications, nor why its victims have met with extreme difficulty in having their adverse events acknowledged and addressed.
Lupron has not only been lucrative for a number of its opinion leaders, spokesdoctors, and prescribers – it has also resulted in a cottage industry born from Lupron-induced iatrogenic injury, requiring acute and chronic office visits and hospitalizations for virtually every practice in medicine (neurology, rheumatology, cardiology, endocrinology, oncology, gastroenterology, psychiatry, pulmonary, dermatology, etc.). This drug isn’t just a “cash cow” – it’s a “cash pig”.
Postscript: Correction
April 25, 2017 – The above is an edited version of an article that was originally published on April 18, 2017. In this edited version, information pertaining to adverse events in one particular pediatric clinical trial has been removed from the original article because this information has been learned to be inaccurate. In the original article, I cited adverse event numbers as found listed within this pediatric study’s results. However, in looking at this study’s list of adverse events, I read (and cited) the reported numbers that followed any particular adverse event – when, in fact, the correct reported numbers were those that preceded any particular adverse event. This list’s reverse order of coding resulted in my (erroneous) conclusion that the numbers of adverse events reported for this trial were in error. (And the list, when read in reverse, provides reported adverse event numbers that exactly match those reported in this trial, indicating no error had occurred.) I have emailed the author of this pediatric study an apologetic note, describing the confusion that resulted from this list’s atypical coding methods, and have acknowledged that the reported adverse event numbers for this trial are indeed “valid”. I apologize to anyone else who may have been inconvenienced by this error.
The original (and now known to be erroneous) text removed from this edited version is included here for your information:
Original Text
CHILDREN: And now, after looking closely at one pediatric clinical trial, there appears to be clear evidence that larger numbers of adverse events were experienced by these children which were not recorded or identified in the final results of this study.
In this pediatric trial, my review counted six adverse events which did not contain the correct number of reported adverse events in the final study results. For purposes here, one adverse event – vomiting – will be used as an example to describe this inexplicable disappearing act of adverse events.
The medical journal publication of this clinical trial, and the ‘study results’ of this trial (housed at ‘ClinicalTrials.gov’) both claim there were “0” reports of “vomiting” in Group 1 (3-month Lupron Depot 11.25 mg) and “4” reports of vomiting in Group 2 (3-month Lupron Depot 30 mg). However, in looking at the history of this trial at ClinicalTrials.gov, which identifies the changes and additions made to this trial, it can readily be seen that the changes made on December 9, 2013 (the additions of reported adverse event numbers) display that for the adverse event of vomiting, Group 1 had “10” reports of vomiting, and Group 2 had “9” reports of vomiting. That is a significant difference in numbers of reported vomiting than is found in the journal publication and in ClinicalTrials.gov study results. And when these documented (but not counted) adverse event reports of vomiting are properly tallied, the claimed incidence of vomiting changes from the published 5.6% to an actual incidence of 26.4%.
In emails to the lead author in attempts to learn the explanation(s) for these missing, untallied adverse events, I was informed that the data as published in the medical journal “is valid” and he is “not the responsible person for this data.” Numerous attempts to learn exactly who is responsible for the data in this clinical trial have proved fruitless to date. How can the lead author not be responsible for the validity of the data from his own study?
Share your Story
If you have a Lupron story, please consider sharing it on Hormones Matter.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on April 18, 2017.
Photo by Pepi Stojanovski on Unsplash.





















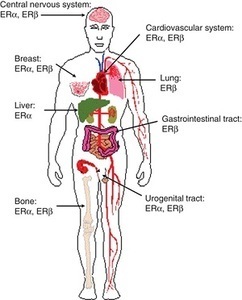 Am I missing some great medical insight that suggests we really don’t need those pesky hormones after all; that all of those hormone receptors located all over the brain and body are there just because? How can a drug like this be used so cavalierly in young women? I don’t have answers for those questions beyond a collective insanity that has permeated medical science where women’s health is concerned. Absent answers, however, what I can begin to provide are data regarding the scope and severity of potential side effects associated with this drug; data gathered from the women themselves, unfiltered by industry bias or potential economic gains. Indeed, I suspect, once the full results of this study are published, industry will be none too happy with me or with our little project. Cue trolls.
Am I missing some great medical insight that suggests we really don’t need those pesky hormones after all; that all of those hormone receptors located all over the brain and body are there just because? How can a drug like this be used so cavalierly in young women? I don’t have answers for those questions beyond a collective insanity that has permeated medical science where women’s health is concerned. Absent answers, however, what I can begin to provide are data regarding the scope and severity of potential side effects associated with this drug; data gathered from the women themselves, unfiltered by industry bias or potential economic gains. Indeed, I suspect, once the full results of this study are published, industry will be none too happy with me or with our little project. Cue trolls.












