Restless Legs Syndrome (RLS), also called Willis-Ekbom disease, is both a neurological and a sleep disorder that is common, but under-recognized. It is characterized by an irresistible urge to move the legs that is worse in the evening or at night. The sensation in the legs is often described as a creepy or crawly feeling in the legs, jitteriness in the legs, or itchy bones. Sometimes the sensation can be painful as well, like a deep ache. The hallmark of RLS is that these symptoms worsen at night or when trying to rest, and the symptoms are relieved by movement. In more severe forms of the disease, the abnormal sensations can also be present in other parts of the body.
RLS occurs in about 7 to 11 percent of individuals, and is two times more common in women than in men. For many people with the disorder, the symptoms are relatively mild, but for individuals with moderate to severe symptoms, it can be quite debilitating, mostly because of the sleep disturbance caused by the symptoms. About 3 percent of the population has RLS with symptoms significant enough to require medical management. RLS is a lifelong disorder and while symptoms may wax and wane over time, they rarely go away completely. Overall, the symptoms tend to worsen with age.
Restless legs syndrome can be primary, meaning that it is not associated with any other conditions, or it can be secondary to other conditions such as iron deficiency and end-stage renal disease. Secondary RLS can also occur in the third trimester of pregnancy. Primary RLS is associated with an earlier age of onset, and often with a positive family history of other family members having RLS. Although all of the mechanisms behind the development of RLS are not fully understood, both iron deficiency and abnormalities in the dopamine neurotransmitter system are involved.
Iron Abnormalities in Restless Legs Syndrome
The link between iron status and restless legs syndrome has been known for over 50 years, ever since the disorder was first described. The lower a person’s iron levels are, the more severe the symptoms of RLS. In order to understand how various blood tests measure and define different types of low iron levels/iron deficiency, some understanding of how the body stores and uses iron is required. Iron is stored in the liver as ferritin, and is released to make hemoglobin in new red blood cells, as required. Hemoglobin is a major component of red blood cells, and is required to carry oxygen in the blood. When the hemoglobin is low (measured by a blood test for hemoglobin or hematocrit), iron deficiency anemia occurs, with symptoms of fatigue, weakness, shortness of breath, headaches, and more. However, even when the hemoglobin is normal, iron deficiency can be present in the form of low ferritin, and this can lead to fatigue and other anemia-like symptoms. One limitation of ferritin as a measure of iron deficiency is that it can be elevated despite low iron stores, in the presence of inflammation.
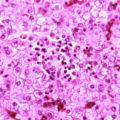
Several studies have shown that giving iron supplementation can improve the symptoms of restless legs syndrome, and in fact, can do so even when individuals have normal hemoglobin and ferritin levels. This is thought to be because RLS is associated with low iron in the central nervous system, rather than low iron in the blood circulation. Although low iron in the blood will result in low iron in the central nervous system, with normal iron levels in the blood (normal ferritin and hemoglobin levels), there can still be low iron in the cerebrospinal fluid, which is a fluid found in the spine and brain. Furthermore, using MRI images, certain areas of the brain have been shown to have low iron in individuals with RLS. Faulty transport of iron across the blood brain barrier has been demonstrated in individuals with RLS, explaining why iron may be normal in the circulating blood, but low in the brain. How this low iron in the brain leads to RLS is not entirely understood, but there is some evidence linking it to the dopamine abnormalities in RLS, which are discussed in more detail below.
Studies of iron therapy for RLS have shown that oral iron therapy can improve symptoms in individuals with low ferritin. However, when ferritin is normal, intravenous iron treatment is required, probably because oral iron is very poorly absorbed. Studies of intravenous iron therapy for RLS (here, here and here) have shown that this treatment is safe and effective, and lasts at least 24 weeks, depending on the type of iron given and the dose.
Dopamine Abnormalities in Restless Legs Syndrome
Levodopa, a drug used to treat Parkinson’s disease, was found to treat symptoms of RLS, at least upon initial use of the drug. Levodopa is converted into dopamine in the body, and therefore it was thought that RLS resulted from a deficiency of dopamine, and thus was treatable with a medication that converts to dopamine. However, brain imaging studies have shown that dopamine is in fact increased in the brains of individuals with RLS. This increase causes the number of receptors for dopamine on neurons in the brain to decrease, something that is predicted given the way neurotransmitters act in the brain, and has been borne out with studies showing fewer dopamine receptors in the brains of individuals with RLS. Levels of dopamine change with the circadian rhythms and are lower in the evening and at night. The increase in dopamine in RLS is compensated for by a decrease in dopamine receptors, leading to an overall balance during the day, but at nighttime when dopamine levels are lower, there is an overall deficit of dopamine activity, leading to the symptoms of RLS.
In addition to levodopa, another type of drug called dopamine agonists are also used to treat RLS. These drugs include ropinirole and pramiprexole; they act by stimulating the dopamine receptors the same way that natural dopamine would. All of these medications have been found to cause something called augmentation, which is when symptoms improve at the beginning of treatment, but over time the symptoms worsen and start happening earlier in the day. This occurs because instead of treating the root cause of the disease, adding additional dopamine to a system that already has an excess of it is actually ends up creating a bigger imbalance over time, decreasing dopamine receptors further.
Treatment Options
In addition to dopamine agonists, other pharmacuetical agents prescribed for RLS include gabapentin, opioids, and benzodiazepines. All of these options have a significant downside, either in the form of side effects (gabapentin), addiction (opioids and benzodiazepines), or augmentation/worsening of RLS (dopamine agonists). Intravenous iron treatment, as discussed above, may be a better option that is safer and also effective. There are also non-pharmacological treatment options that have been shown to ease symptoms in some individuals. These include moderate exercise, leg massage, hot baths or heating pads, and a regular sleep schedule and avoiding naps. Avoidance of lifestyle and diet factors that may worsen symptoms can also help–this includes avoidance of alcohol, nicotine, and caffeine. Finally, some medications can worsen RLS, and these should be avoided if possible: antidepressants, anti-psychotics, diphenhydramine (Dramamine), and dopamine antagonists used to treat nausea and vomiting, such as metoclopramide. In many individual combining non-pharmacological approaches with iron therapy may make symptoms manageable.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
This article was published originally on January 11, 2017.














Copper helps make iron useable from stored cells. I make sure to have oysters. Made huge difference to iron levels when eating meat or iron supplements did nothing.
Also if I still have restless legs the other thing that works is Niamacide , just a pinch. Knowing this has changed my life. I have zero restless legs and I would say at one point it was so suffer
RLS is yet another manifestation of energy deficiency and Ali is quite right about garbage in the American diet. Get rid of sugar and high calorie malnutrition. Note the benefit from magnesium. This mineral and thiamine are together vital to energy production, so if you have RLS, try getting rid of sugary junk and getting thiamine and magnesium in large dose supplementation.
So sorry for your horrible experience! One cause of RLS is actually iron dysregulation; too much iron is stored in the tissues but cannot be accessed by the blood and body where needed. Read Dr. Morley Robbin’s Root Cause Protocol (www.therootcauseprotocol.com) to learn of the importance of balancing copper, iron, magnesium and ceruloplasmin in the body.
His new book, [Cu]re: fatigue, is excellent. It describes how iron overload is the chief cause of all inflammation in the body and simple steps to overcome it. You are making yourself worse by taking even more iron. All the best to you.
Years ago I read in a doctor’s Q&A column carried by our local newspaper of a professor, who experienced restless leg syndrome throughout the day, and resolved it by carrying small bar of soap in his pants pocket. This medical columnist heard frequently from people who slept with a bar of soap in their bed sheets to resolve, or lessen their RLS symptoms. Apparently, it is the magnesium in bar soap that can help. I take various forms of magnesium (glycinate, malate, etc.) orally, throughout the day, plus slip a sliver of soap into my stockings/socks before attending concerts that will require long periods of sitting. If I keep on top of it, my symptoms are greatly resolved.
Dr. Bridge-Cook,
Hi there. I’m a journalism student and freelance reporter, and I’m working on a story about how women’s pain is often dismissed and treated differently from men’s. I understand that endometriosis is a common cause of pain that’s not taken seriously by doctors, but I know there are others. I read your bio here, and I wonder if you’d be willing, or if you could put me in touch with another woman who might be willing, to talk to me about a negative experience in the healthcare system caused by pain or other symptoms not being addressed well. I’d sure appreciate the chance to hear and share the story of someone who’s been through that.
I won’t take more than 20 minutes of your time–unless you’re willing to talk longer, in which case, of course, I’m happy to listen.
Thanks very much!
Hi Brett, I’d be happy to talk to you. You can contact me through info@endometriosisnetwork.ca.
If only GP’s and doctors were all forced to read this. RLS is quite literally killing me. I was on dopamine agonists for 15 years and they worked brilliantly until the dreaded augmentation occurred. I went through 2 solid months of withdrawal hell getting off the dopamine agonists with RLS in every part of my body and unable to sleep/sit still for longer than 10 mins at a time. Trying to find drugs to control it now is impossible. I’ve tried gabapentin but it stopped working and am now on opioids which aren’t really helping. The nightly torment of this disease is like torture and like many others with the severe form of this disease, I’m not sure how much longer I can go on. I haven’t touched caffeine, alcohol, chocolate, sugar or gluten and been very low carb for months in desperation to try to make it stop. My ferritin levels are above normal ( I’ve been taking ferrous bisglycinate for months) but not sure how I can convince a neurologist to give me an iron infusion if my ferritin levels read normally. If anyone knows of a GP/neurologist giving iron infusions to help severe RLS cases please post details.
Julie are you on Facebook as there are a couple of excellent support groups Nightdancers and Restless Legs Syndrome Sufferers. I know of 2 Neuros who do iron infusions in the UK. Dr K.Ray Chauduri Professor of Neurology at Kings College Hospital London and Dr Kirsty Andersonat Newcastle Hospital
Dumping wheat & gluten and going very low carb got rid of my RLS. I believe there is a gut connection to this, as some nerves to the legs run down by the bowel. I also had other issues including early neuropathy, characterised by burning feet and needle pains in my toes. All that rectified on GFLC also. I believe that modern wheat and other low nutritional foods like sugar and processed garbage rob far more nutrition out of the body than they ever give it. If essential elements needed for its digestion and processing within the body are denatured or missing, the body then has to steal them from itself in order to complete the process. Once a food enters the stomach, the body has no choice but to have to process it……