If you have severe Atopic Dermatitis I am going to guess your story. It probably started when you were a child with a small skin patch that was very itchy, and the doctor prescribed a steroid cream to cure you. ‘Wonderful,’ you thought, ‘now I won’t have to worry about this anymore.’ But soon the eczema returned, only now it had spread a little more. So again you proceed to apply the steroid cream, and again, it heals as if by magic. Eventually though, the rashes come back, and they’re also getting worse. They are itchier, swollen, red, and maybe, even painful.
Your doctor also encourages you to start using moisturizing creams, the more expensive the better. At this point you may have had to move on to stronger steroids or perhaps even a topical immunosuppressant (e.g. tacrolimus). You no longer remember your life without dermatitis. Creams do work, but only to a certain degree. You have to start considering new options: light therapy, strong antihistamines, and more and more moisturizing creams. Your doctor may even have mentioned the possibility of trying oral immunosuppressants by now. ‘Immuno… what?’ you whisper to yourself. ‘But I only have dermatitis. When did it turn into all this!?’ The disease has begun to affect your daily chores, your personal relationships and your psyche as well. Meanwhile, you continue to religiously comply with your doctor’s instructions, buying every cream, taking every antihistamine and wishing to one day just be cured.
‘And now what?’ Now, two paths open in front of you: you can keep following the conventional medical system path, adding new drugs and treatments that promise you the same results as that very first steroid cream many years ago, or you can take matters into your own hands and try to find out what is really happening inside you.
The Search
I’ve always been a very curious individual. One of the reasons I decided to become a researcher is due to the fact that I don’t ever stop asking questions. When the subject of study became myself, I used all the tools in my shed to get to the bottom of what was happening inside my body. And so, with the help of my scientific mind, I decided to start looking for alternative views, different opinions and new theories about my illness. I read every paper and scientific article I could get my hands on and spoke to dozens of people going through the same thing. Until one day, while casually watching YouTube, I came across a video called “Topical Steroid Withdrawal”.
‘Hmm, how strange’ I thought to myself. I had been using topical steroids for years by then, and had never been told about any side effects. Filled with curiosity and excitement about this new hypothesis, I decided to start investigating, and soon I found the International Topical Steroid Awareness Network page.
Suddenly, something clicked. I did not have atopic dermatitis. I was, in fact, suffering from the side effects of the number one treatment for atopic dermatitis, which is a disease in itself: Topical Steroid Withdrawal Syndrome (or Red Skin Syndrome, or simply TSW). Being able to finally pinpoint the source of all my suffering felt like a weight had been lifted off my shoulders, and gave me a sense of relief I truly hadn’t felt in years. Little did I know the real struggle was only about to get started.
What Exactly Is Topical Steroid Withdrawal Syndrome?
As its name suggests, TSW means that you are in the process of withdrawing from a drug; in this case, topical steroids. You can be in withdrawal even if you’re still using the steroids. In fact, that’s the reason why you need higher-strength steroids every time you visit your doctor. Your skin rapidly got addicted to every new prescribed steroid, and every time you tried to discontinue it, you began the withdrawal period. After some time, not even the strongest one can manage to contain the withdrawal effects.
Withdrawal from corticosteroid creams is different from other withdrawals because it begins in the skin and then moves to the rest of the body. When Dr. Kenji Sato, one of the Japanese doctors who discovered this syndrome, observed portions of skin under the microscope after intensive use of topical steroids, he discovered that the skin had been atrophied and could no longer function properly. And that’s where everything starts to go wrong. When your skin starts breaking down, your immune system loses its first barrier of defense. What this means is that many new and foreign particles can now enter the skin and eventually end up in your bloodstream, putting your whole body on high alert. In response, the body begins to release inflammatory chemicals like histamine to protect you. Normally, inflammation is supposed to subside after the invaders have been ‘contained’, but in our case, the skin is so broken that the body can’t keep up with all the new allergens, making us hypersensitive to everything. The skin begs to be closed again, so it establishes a healing mechanism by peeling and drying. This is one of the reasons why moisturizer withdrawal (MW) and no moisturizer treatment (NMT) work very well, even on normal eczema.
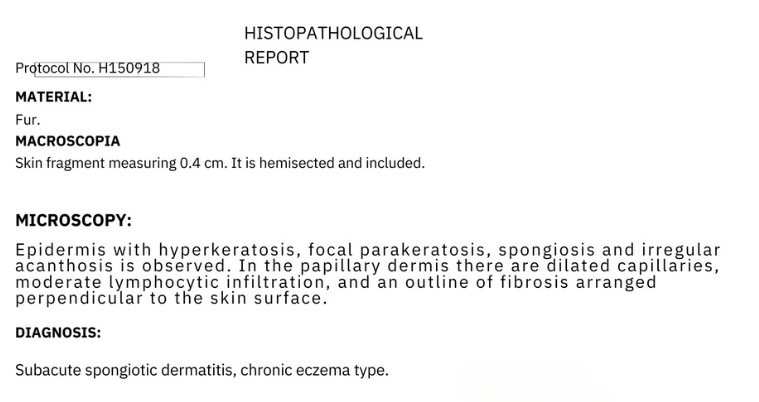
Skin atrophy can manifest as dry, cracked skin, but this also has its counterpart in the form of vasodilation. Topical corticosteroids work by constricting blood vessels, which reduces the amount of blood in the skin. When you discontinue them, the immediate reaction of those blood vessels is to open up again, which causes oozing, redness and itching. Vasodilation is probably one of the worst symptoms of this disease. In fact, it’s what gives TSW its medical term: Red Skin Syndrome. Unfortunately, not much can be done to alleviate it. Moisturizer withdrawal, ice-packs, fasting, NSAIDs and LDN (in some cases) seem to reduce inflammation somewhat, but it will still come and go until the blood vessels heal and the skin learns to function without steroids again. While skin damage can be easily seen under a microscope, in my experience it is useless to have a biopsy done because doctors still cannot identify the cause. Corticosteroids do not last long on the skin, but the damage they cause does.
What Is the Difference Between Dermatitis and TSW? Does Severe Atopic Dermatitis Exist on Its Own?
This is just an observation, but personally all the cases I have seen of moderate to severe atopic dermatitis that had their onset after the use of topical steroids are in fact unrecognized cases of TSW. The explanation lies in the very concept of dermatitis. As Dr. Marvin Rapaport (a reference in this community) explains, dermatitis or eczema is characteristically a childhood disease, which develops in response to an allergic environmental or food stimulus, and which should resolve spontaneously without major consequences. In no case whatsoever will a disease like dermatitis cause widespread outbreaks that burn, become inflamed or look very red, or that itch so much that they keep you up at night. If you are experiencing something like this and have recently stopped topical corticosteroids, you can be almost certain that your body is going through phases of addiction/withdrawal (i.e., Red Skin Syndrome or TSW).
Conversation #1 With Dr. Marvin Rapaport.
Red Skin and Topical Steroid Withdrawal
‘And why won’t my doctor tell me!?’ Simply because they don’t know. As Rapaport states, dermatologists nowadays, especially the newer ones in this field, have lost the ability to recognize and identify TSW since they have never seen cases of “normal” dermatitis to contrast them with. Given the abusive treatment with topical steroids for any minor skin problem, they are now facing thousands of cases of corticosteroid-induced dermatitis, which they will simply call “moderate to severe dermatitis”. Trying to talk to them about this is in most cases useless. Since it is an iatrogenic disease (that is, literally caused by doctors), recognizing the existence of this syndrome would mean a legal problem for them. There is also no research on this, because Pharma is not interested in financing these types of studies since there is no real solution that they can sell you.
So What Can We Do To Feel Better?
Best advice is to treat TSW the same as the classic old-fashioned dermatitis: eliminate ALL commercial cosmetic products (and that includes moisturizers), and look for natural alternatives for everything. One of the easiest and most effective things you can do is immersion baths with baking soda, apple cider vinegar, sea salt or Epson salts, and moisturizing with shea butter, coconut oil or aloe vera if you are not willing to do MW.
Additionally, it would be a good idea to pay close attention to your diet. Whether vegan, paleo, keto or carnivore, the most important thing is to try to eliminate all artificial products, especially ultra-processed foods containing preservatives, flavorings and additives, because they will end up in your blood and put your immune system on alert again. Be mindful of fruits and vegetables since they are the ones that tend to cause the most allergic reactions. If you feel you could use some extra help, consider adding supplements as well. I have found that vitamin C, high-quality collagen and zinc are the top three for healthy skin.
Above all, you will need tons of time, patience, and confidence in the thought that there is an entire community present, struggling with the same syndrome, willing to provide support and help.
Where I Am Now
It has been exactly 1911 days since I completely stopped steroids (but hey, who’s counting?). In the past 5 years I have gone through a physical and emotional rollercoaster like no other. Funny thing about TSW sufferers is that we hate being seen, but we take thousands of selfies. I never thought I would actually share them with the rest of the world, but I guess I am finally coming to terms with this part of my life.

After a year of dealing with this on my own, I decided it was time to go back to my doctor and ask for help. She was horrified by the state of my skin and of course blamed me for letting my eczema get this bad. Soon I was offered a plethora of medical treatments, and after a lot of thought, I decided to accept Methotrexate -an immunosuppressant used for some types of cancer and some inflammatory diseases like arthritis and severe dermatitis-. After 9 months of use, I wasn’t seeing any major effects on my skin, and the side effects like fatigue and hair loss were starting to kick in, so I decided to call it quits.
By July 2022, I was already 3 years into TSW and my skin wasn’t as angry or itchy anymore, but my sensitivities and allergies were still out of control. That is where I was introduced to a relatively new drug called Dupilumab (Dupixent), which is an immunomodulator designed specifically for people with eczema. It is not the miracle drug they usually make it out to be, but it has definitely been helpful. I also started focusing on my mental health, began exercising, found a good diet (that was a rollercoaster of its own), moved from my childhood home, finished my studies and found a life partner.
This is me today at age 25.

Whenever I look back on my early 20s I always think about how rough they were, but also how mentally strong I was and how much I’ve learned and grown, and how I wouldn’t want it any other way.
So goes life.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Share Your Story
If you have experience with atopic dermatitis and/or topical steroid withdrawal syndrome, share your story. Send us a note here for more information.














My wife had TSW. Technically probably still has it but it is much improved. Finally. After nearly 4 years of it. Believe me when I tell you I became a research hound over this condition. She was an absolute mess and it really destroyed everything about her life. What I can seemed to help her the most was juicing carrots. Daily. 16 ounces of fresh carrot juice, spilt up into 8 ounces twice a day. She also saw a near immediate improvement by eliminating fermented foods…aka pickles, anything with vinegar aka ketchup, mustard, sauces, ranch, hot sauce etc…these always inflamed her neck/mouth area.
I do actually think there is an EMF element to this. And even though steroids play a role in destroying the skin and depleting all kinds of nutrients, the damaged skin is probably further damaged and less protected from EMF, thus creating a loop of dysfunction….EMF damage causes more inflammation, and inflammation damages the skin more…on and on. That’s my theory anyway…which would also explain why TSW is becoming more and more widespread here in the past few years.
This was my son. Eczema started at weaning at 7 months and got steadily worse. By the age of 2 he had had two or three lots of antibiotics for infected and weeping skin on his face – I remember the misery of the night his face was so bad he woke literally every 30 minutes with the pain of it. He was an allergic child – he had about 15 IgE allergies and (we later discovered) intolerances to just about every natural food chemical going, as well as artificial ones.
He was given moisturisers and topical steroids, with increasing strength, and also topical immune suppressing creams. By the time he was 20 months old, he was on adult strength steroids, which were not licensed for children under 2 – the pharmacy interrogated me about it every time I picked up a new tube. I had to apply moisturiser all over his face & hands before each time he ate, and wash them again with a different moisturiser after eating to remove any food particles from the skin. He had to wear anti-scratch mittens at night and sleep on special sheets to stop his skin sticking to the bedding. Even with that, his eczema was still awful, and whenever we stopped using the steroids, it became massively worse. We kept him obsessively out of the sun because the immune suppressing cream was known to have carcinogenic effects if the person had lots of sun exposure. (He later turned out to have significant vitamin D and therefore calcium deficiency as a result.)
His dermatologist retired and we were assigned to a new one. At the first appointment he told me that my son was suffering from steroid withdrawal and that we should go cold turkey on the steroids. I was extremely resistant because I knew how bad his skin got when we stopped using it, but the dermatologist insisted. He gave us increased strength topical immunosuppressants but apart from that it was just a case of going cold turkey.
The next few months were dreadful, but he was right: after getting the steroids out of his system, his skin really calmed down and the intense & infected patches did not recur. Almost all the misery we had endured had been due to the steroid medications.
Once things had calmed down, he still had eczema, but we didn’t use any treatment on it at all. I soon discovered that his skin reacted to the foods he ate. I asked his dermatologist, who said that food had no connection with eczema, but I had worked out exactly how to produce an eczema flare by feeding him the ‘wrong’ foods. He ate a low sugar, natural wholefoods diet, but still many foods caused his eczema to flare up and I worked out that he had problems with gluten, dairy, salicylates, phenols, glutamate, so-called sulphurous foods, tyramine and histamine.
We later found out that he had multiple nutritional deficiencies – B vitamins, especially B1, B12, iron, zinc, selenium and others. Fixing those brought massive improvements in skin and food toleration; benfotiamine and then TTFD fixed the overt beri beri symptoms he still had whilst taking high dose thiamine HCl. Today at age 14 he hasn’t had eczema for years, and the only category of natural wholefoods we have to avoid is gluten.