I am 45 years old with a history of “undetermined post-viral effects” since March 2020. It is not clear what virus was in question originally, but Epstein Barr and cytomegalovirus have been flaunted due to the high lab titers of those two. As far as I’m concerned there are too many of them out there to find an exact pathogen that caused it. Moreover, the symptoms overlap and there is no treatment available that would be tailored to any specific one.
I also have a history of heavy drinking in my youth, a habit I dropped 8 years ago and have since cleaned up my act. This is worth mentioning because it may have caused susceptibility to illnesses that should be relatively harmless. My full health story can be found here: Recovery From Alcohol Induced Gastric Beriberi and Dysautonomia – Hormones Matter.
I began high-dose thiamine therapy in October 2020 and have benefited outstandingly. Aside from a period in 2021 when I stopped taking thiamine altogether for three months, I’ve been able to maintain relatively normal health status and keep symptoms of dysautonomia at bay with a variable dose of 300-500 mg of TTFD a day.
Over the year 2022, I became increasingly drowsy several hours after my dose and I experienced various symptoms of osteomalacia. My primary care doctor referred me to an orthopedist doctor who ordered an MRI of affected joints/bones and concluded there was nothing there to be seen. He recommended steroid injections. I felt odd about it because I seemed to now injure myself with the slightest bump and exercise. As a result, I became more sedentary.
I googled my symptoms and the search suggested rickets and a possible vitamin D deficiency-related cause. This was dismissed because my symptoms were eerily similar to the beriberi I developed previously. Also, I didn’t look malnourished and my vitamin D was in the normal range. Rickets can be a result of increased phosphate excretion, a connection I found later when studying acid-base disorders. I suspected this was the case for me.
By accident, I discovered that thiamine inhibited an enzyme called carbonic anhydrase. Carbonic anhydrase inhibitors, like the drug acetazolamide (Diamox), are used to treat altitude sickness and intraocular pressure. Inhibiting this enzyme increases carbon dioxide retention, which paradoxically, aids in oxygenation. It does this by triggering CO2 sensors in the kidney tubules, which in turn alert the brain for increased breathing. This state of the body is mildly acidotic because the acidosis is achieved by increased excretion of alkali salts – bicarbonate, potassium, phosphorus, calcium, and sodium.
Acidosis and its counterpart alkalosis are shifts in intracellular/blood pH that can be either a result of breathing (respiratory) or kidney excretion (metabolic). Drugs can induce either state.
In drug-induced acidosis, the body attempts to fix the imbalance given there is an adequate supply of buffer ions at hand, such as bicarbonate from food (think fruits and vegetables). If that supply runs low, the necessary buffer is leached from the bone reserve. In the long term, this will cause osteoporosis, the first stages manifesting as bone pain. Increased phosphate excretion also causes dips in bone reserve to replenish the necessary electrolyte supply. The human body is smart. This constant acidosis is what I perceive happened when I began experiencing bone pain and drowsiness.
Renal Tubular Acidosis Type 2 as a Feature of Long-Term High-Dose Thiamine Therapy
High-dose thiamine users know how thiamine increases urination. This is a positive effect because it also alleviates edema and swelling. The downside is the loss of electrolytes. The need to balance electrolytes with acute thiamine repletion is well known, however, the potential for electrolyte loss is less well understood with the use of high-dose thiamine for longer durations. Much of the literature assumes short-term high-dose use, but individuals with chronic illness are likely to supplement thiamine for long periods and here there is little guidance. This is where I found myself, experiencing phosphate loss, which led to an exacerbation of my original symptoms plus some new ones, including a low-grade state of acidemia.
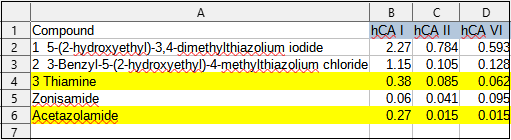
Technically, thiamine treats acidemia. Thiamine deficiency is a noted cause of excessive acid, but I was already taking thiamine, so this was perplexing. Why would I become acidemic? I believe it because the mechanisms are different. In thiamine deficiency, acidosis is caused by an inability to metabolize pyruvate in the mitochondria and thus much of it is converted to lactate, which builds, and eventually contributes to lactic acidosis. In the case of long-term high-dose thiamine, however, the altered acid/base balance evolves from the inhibition of the carbonic anhydrase enzyme coupled with insufficient electrolytes, particularly phosphate. Carbonic anhydrase inhibition, by design, causes acidosis and a great deal of renal bicarbonate wasting. Absent sufficient electrolytes, long-term, high-dose thiamine may also cause slight acidosis/acidemia. The table below illustrates how thiamine inhibits the carbonic anhydrase enzymes. When compared to the most popular carbonic anhydrase inhibitor drug, acetazolamide, thiamine induces 50% to 400% more inhibition depending on the enzyme’s isoform.
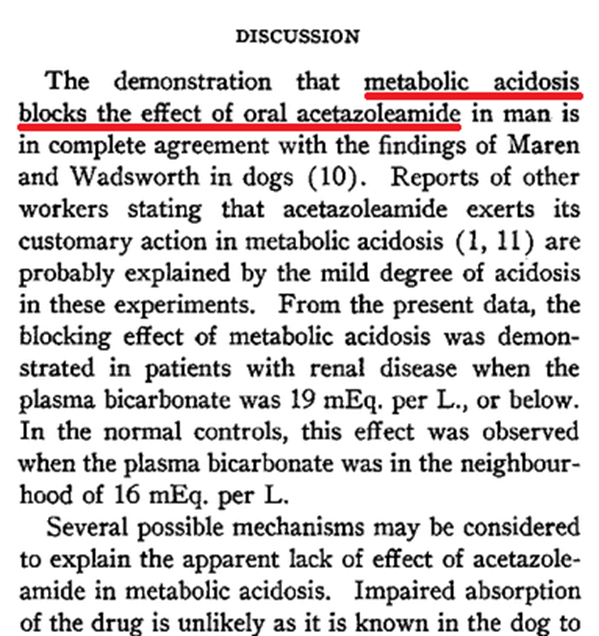
In a similar vein, it is proposed that this prolonged low-grade acidosis is the reason why acetazolamide stops working and requires time off. The self-limiting effect of acetazolamide was described as early as 1957 in a paper by Campbell et al.
I believe the prolonged inhibition of carbonic anhydrase and subsequent loss of phosphate ions may also contribute to the diminishing effects of thiamine observed over time.
Did I Really Need More Thiamine?
When I became severely acidotic, I felt the effect of thiamine diminishing and so I added more thiamine, thinking this would improve matters. After all, thiamine is known to correct acidosis. I added benfotiamine every 2 hours until I was at 2200 mg a day of benfotiamine and 500 mg a day of TTFD. My symptoms were barely manageable. As I didn’t know what was going on, I believed I was struggling with additional stressors that required more thiamine to resolve. This had happened before and resolved on its own when I had a head cold or other life stressors. I tried to stay calm and reasoned that if this requires more thiamine, no worries. I’m giving the body what it wants. I always felt relief after dosing, which encouraged me to think it was a lack of thiamine, not something hindering the effect. The doses were alarmingly high compared to my normal maintenance dose of 300 mg of TTFD.
When I connected the dots between thiamine and its effect on carbonic anhydrase and the acid/base balance, I decided to stop taking thiamine for a period to flush everything out of my system. According to the research on acetazolamide, during the flushing period, acidemia is generally self-correcting, and when therapy is resumed, it is likely to work again. With acetazolamide, acidemia is both the feature, the consequence, and the self-limiting factor.
Similarly, Dr. Costantini whose clinic has made groundbreaking progress in treating patients with Parkinson’s disease, also advises taking a few weeks off from the high dose of thiamine every 3-6 months. They have not elaborated on the reason, possibly because it is not widely understood. Perhaps it has just shown to be effective in long-term treatment.
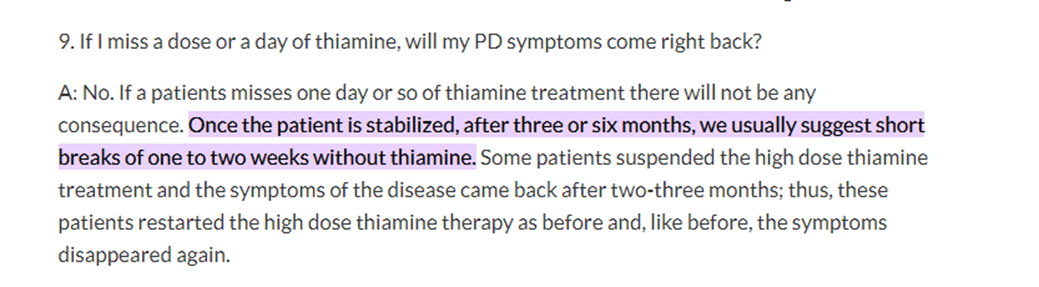
Figure 3. An FAQ from Dr. Costantini’s website.
Unfortunately, for me, when I ceased taking thiamine, I experienced a rapid return of all of the original symptoms of dysautonomia that precipitated its use in the first place. I simply cannot habitually take days off to allow for pH balancing (and I am not sure how Constantini’s patients were able to do so). I had to find another way to manage this. I also learned that another staple supplement I used to take, potassium chloride, to prevent potassium deficiency, may have also contributed to a higher acid balance. Hyperchloremia, too much chloride, is mentioned frequently when I read about renal acidosis related to bicarbonate wasting. In medical lingo, this is called medically induced renal tubular acidosis type 2. I since have switched to potassium bicarbonate.
Correcting Thiamine-Induced Renal Acidemia
For me to correct the renal acidemia, I required a bicarbonate supplement. This was partly because I had used such heavy doses of thiamine that my acidotic symptoms were already rather severe. Had I intervened earlier, I would have relied on bicarbonate sources in the diet, aiming for 20 mEq or so a day (see below). My phosphate intake from meats and dairy was more than adequate but again the degree of acidosis has likely caused more phosphate wasting than I could compensate for. That is why the initial provision for bicarbonate supply has been my chosen method of correcting the balance.
As I mentioned previously, when I ceased taking thiamine, I developed a headache that would not respond to NSAIDs and intracranial pressure which landed me in ER. I came back home with vertigo, shivering, and unsteady gait, with a prescription for corticosteroids and an inconclusive CT scan result as a souvenir. I took more thiamine and returned to baseline in an hour.
I began sodium bicarbonate that night and felt instantly more clear-headed. It was like a weight had been lifted off my shoulders. I corrected too aggressively over the next two days and possibly experienced paradoxical CNS acidemia as a rebound, with somnolence and nausea. Instantly though, the thiamine felt super-charged and I needed only a fraction of the dose I need previously. From there, I began a conservative bicarbonate supplement routine and now after four weeks, I am in a comfortable place of moderate TTFD (300 mg) and morning plus evening potassium bicarbonate of ½ tsp, providing 20-25 mEq bicarbonate and 1200 mg of elemental potassium for each dose. I arrived here from ¼ tsp twice a day and every week raised it a little.
I feel overall much more clearheaded. I don’t have the stuffy foggy feeling that would first go away with more thiamine and then return shortly after (which made me think I needed more thiamine). I have returned to my maintenance dose after having gone almost ten times higher when it had stopped working. I assumed the developing symptoms indicated an increased need for thiamine when in reality it was an increased need for phosphate.
Dietary Contributors to Acid Balance
For most people, a balanced diet should contribute to a healthy acid/base homeostasis. Poor diet and/or high dose thiamine may shift that balance if one is not careful. According to an online source of the potential renal acid load (PRAL) of foods, meats, cheeses, and grains tend to contribute to renal acidity whereas fruits and vegetables contribute alkali ions. 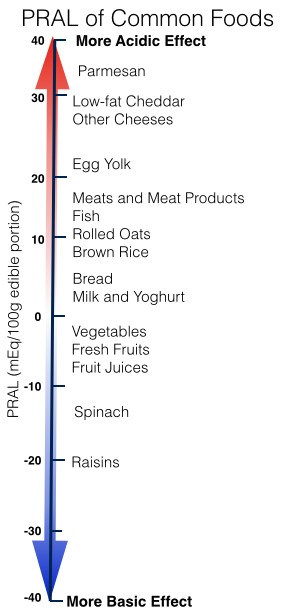 Vinegar and citrus fruits provide a weak conjugate of acid which turns to bicarbonate and supplies alkali ions but the amount is too small to rely on exclusively. Inconclusive studies have been done with citric acid (lemon juice) and potassium citrate as oral alkalinizing agents in the ambulatory setting. Lemon juice may simply fine-tune the system, but the math suggests one would need an awful lot of lemon juice to make a significant difference in acidity.
Vinegar and citrus fruits provide a weak conjugate of acid which turns to bicarbonate and supplies alkali ions but the amount is too small to rely on exclusively. Inconclusive studies have been done with citric acid (lemon juice) and potassium citrate as oral alkalinizing agents in the ambulatory setting. Lemon juice may simply fine-tune the system, but the math suggests one would need an awful lot of lemon juice to make a significant difference in acidity.
Conclusion
To sum up there are several types of acidosis and while thiamine definitely helps with the lactic one, it quite possibly causes the renal one. Knowing the difference may allow one to navigate long-term thiamine therapy more effectively. It may also help explain some of the negative effects noted with thiamine repletion.
Bicarbonate repletion is appropriate in the type of acidosis that is caused by depletion of a buffering agent. In diabetic ketoacidosis or lactic acidosis it is not beneficial. Those types require a different approach.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Kidney Lake, Rila, Bulgaria. Photo by Yuliyan Grozdev on Unsplash.
















I wonder if metabolic acidosis is the mechanism behind high dose thiamin leading to increased blood pressure.
https://pubmed.ncbi.nlm.nih.gov/33374943/
Thank you, Linus, for sharing this! My 300mg daily lipothiamine had slowly begun to stop working by about 10%, but I took 1/4 tsp of baking soda a couple hours ago and I’m feeling so much better. This explains why after a trip during which I took extra thiamine, all I wanted to drink for a couple weeks was Evian, a high-bicarbonate water I normally find to taste bitter and unpleasant! I’m so happy to be able to head off these returning thiamine deficiency symptoms before they got bad. Thanks again!
This is fascinating. Linus, what do you think of taking potassium phosphate instead of potassium bicarbonate?
Regardless, I will try your same experiment because I have been taking high dose thiamine HCL since late 2021.
Also, how can we follow you on this and other forums?
Linus,
Thank you for the article. How are you doing today with taking bicarbonates?
Hi Linus! Can you clarify how you ended up fixing this issue? I am a little confused by the third paragraph under “Correcting Thiamine-Induced Renal Acidemia.” Did you take baking soda (how much?) the first two days? And then switch over to a potassium bicarbonate powder supplement? Great job figuring this out!!
You mentioned intracranial pressure – I’m curious if you had a lumbar puncture done to confirm this. Your experiences seem eerily similar to what I’m going through. Please email me if you have the time; I’d love to compare notes on some things.
I wasn’t tested because two years earlier I had an MRI which was clear. This rendered me completely healthy in the opinion of my neurologist.
I went to urgent care with bulging eyes which periodically teared up, relieving the pressure for a moment and again I was told maybe I have “eustachian tube dysfunction” because of the dizziness involved. It was like shouting into a void.
Fantastic information, thank you for sharing. I dug myself out of a lifelong chronic illness hole by fussing with nutrients for years, and along the way I have observed so many double-edged sword reactions in myself and others. Mineral imbalances make such an enormous difference to how things function in the body. It can be quite dismaying to know that a nutrient is clearly making an enormous positive difference yet something has suddenly thrown a wrench in its function. I’m glad you figured out what was going on in your case and wrote about it.
You are already maintain the dose of 300 mg TTFD right ?, do you have a plan not to use TTFD in the future ?
I need to use TTFD possibly for the rest of my life. It’s a minor inconvenience compared to the debilitating illness I had – now if I can manage the downstream effects on electrolytes with modest bicarbonate supplementation, I’ll be happy and hopefully healthy!
My journey of using TTFD is same to you, i have start the protocol around Feb/2022 .and the highest dose of thiamine i have use is around 700 mg ttfd, 700 mg benfo. I think have the problem of acdosis and start 600 mg sodium bicarbonate and feel good overall.To know exactly, I have tested my urine and it show way to acidic (ph ~ 6).A very outstanding post, wish you all the best
That’s great!
I’ve not established whether it would be good to just pulse bicarbonate or stay on it. Maybe you find out. Please come and tell your progress.
I will update my progress in this post after 2~3 weeks when i know exactly how to titrate the bicarbonate dose. By the way i am already read the book : https://www.audible.com/pd/Sodium-Bicarbonate-Audiobook/B07CYPNZ3S
Hope you find good information .
One thing you might want to consider is urine pH in the context of taking thiamine. The acidosis from bicarbonate wasting should yield a steady alkaline urine pH, an indicator that bicarbonate is, indeed being excreted in high amounts.
I’m not sure why your urine pH would be acidic in that context – unless you’re taking a break from thiamine while repleting bicarbonate pool.
I’ve got no benchmark of my own, I didn’t come to think of testing urine pH while in having symptoms of acidosis, so I can’t contribute to how it’s reacting now.
Translation types
Text translation
Source text
1,313 / 5,000
Translation results
I always thought: there is one optimal number for all tests. as in this case, I am reading a lot of scientific papers to find those optimal numbers (urine ph and I don’t understand how you can tolerate 1200 mg of potassium bicarbonate with no side effects, my mother only took 300 mg of sodium bicarbonate and had an immediate rise in blood pressure (my mother also taking thiamine but about 50 mg a day for 5 months), in my case I only took 200 mg of potassium bicarbonate and 100 mg of sodium bicarbonate , I checked my urine pH was greater than 6.5 (if I I took >300 mg of potassium bicarbonate and my heart felt a little tired). The strange thing when I supplemented with bicarbonate was that it made me have more bowel movements (I had to stop taking thiamine in the past because it made me have a bowel movement at first. extremely good but later causes constipation). Currently I can tolerate about 100 mg of TTFD and maintain normal bowel movements, there are a lot of things. Welcome and I will continue to update.
Regarding your argument: Acidosis due to bicarbonate excretion will produce a stable alkaline urine pH, I think it is only correct in the first stage when using b1, but later when bicarbonate is depleted, the body will definitely fall. into an acidified state (shown by the pH of saliva and urine)
i just want to leave you to know magnesium is sodium antagonist ….so it would be a good idea take high magnesiun dose white you take bicarbonate
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1751-7176.2011.00538.x
It is my understanding that mineral citrates like Potasium Citrate and Magnesium Citrate are quite effective at clearing extra and intracellular acidity. Personally I would be quite wary of bicarbonate supplementation due to its effect on lowering stomach acidity – which does not happen with the citrates.
Do you or anybody have any experience with potassium gluconate? Would it too help clear intracellular acidity I wonder?
Thank you for the great post. Could I connect with you vis email Linus? I am a physician that has seen a similar supercharged reaction to Thiamine after addition of a base. Until I read this article I never made the connection. Thank you.
Very interesting, and helpful. Thanks so much for sharing your experience and your research! So pleased for you that you figured this out.
When looking into lipothiamine supplementation (for POTS) recently I noticed people seem to like it supported with an electrolyte combination of magnesium taurate plus potassium bicarbonate (for example the Cardiovascular Research/Ecological Formulas combination). I wondered at their choice of bicarbonate there versus other forms of potassium but I guess this may help prevent against renal acidosis when taken from the outset?
I’m going to read your previous article now. Thanks again for sharing your story!!
Potassium bicarbonate seems to be more widely available now, and that’s indeed what I take now. I had not understood that potassium chloride (salt substitutes in grocery store) was contributing to acidosis, since chloride burden was exacerbated already.
How much potassium bicarbonate do you take? and can we take it with food together with other supplement? as it can reduce the stomach acid?