Our Kids Are in Ketosis
Some time ago, I published an article on Medium titled “Our Kids Are In Ketosis”. The article turned many heads and has been shared thousands of times on social media. It has also been cited by an MD in a YouTube video here. So what is the fuss about?
Various ways of eating are labelled as “diet fads” by many people, including many doctors, scientists, and nutritionists. A fad is defined as “an intense and widely shared enthusiasm for something, especially one that is short-lived and without basis in the object’s qualities; a craze” (Google dictionary). Some diets should be labelled fads because it is impossible to maintain them long term. Fruitarian, for example, is one such fad; it is impossible to maintain safely long-term by humans, primarily because one may die from starvation, pancreatic cancer, or as a result of insufficient nutrients in a diet that contains only fruits. In addition to the demand that is placed on the use of insulin to remove the glucose oversupply from the blood, fruitarian diets lack essential amino acids and essential fatty acids for survival.
Some may suggest that the Standard American Diet (SAD), also referred to as the Western Diet, is a fad. The majority of the US population consumes the SAD diet with dire outcome: heart disease, obesity, type 2 diabetes, non-alcoholic fatty liver disease, cancer, Alzheimer’s disease, multiple sclerosis, Parkinson’s disease, nearly all (if not all) autoimmune diseases, and a host of other non-communicable diseases are outcomes of the SAD diet. While on a human life scale we may think of the SAD diet as sustainable, it clearly is not. It has been on the menu for over 50 years, and it feels awkward calling it a fad, even though it most certainly meets “without basis in the object’s qualities”.
“Let food be thy medicine, and let medicine be thy food”
This wise sentence is attributed to Hippocrates. As ancient as this statement is, it still holds true today—if only we followed its wisdom. I am a follower of another Hippocrates saying with a slight modification: “You are not what you eat but how you metabolize what you have eaten!” You will find this sentence as my intro (mission statement) on my FB page. The distinction between what we eat and how we metabolize what we have eaten is essential; it defines who we are.
Understanding Diet and Nutrition
In order to understand how nutrition affects us and what we should be eating, much needs to be understood about the human digestive and metabolic systems. While there is a lot of discussion about the importance of carbohydrates in our diet today—particularly consuming many servings of complex carbohydrates, such as whole grains, starchy vegetables, and fruits daily—this was not always our understanding. For example, when I grew up, carbohydrates were understood to cause obesity(1). Most of my childhood was spent on a relatively low carbohydrate diet—and that was normal for Europe at that time. Cereals—whole grain or otherwise—didn’t exist, neither was I growing up drinking orange juice and eating pancakes with syrup in the morning. In those years, the role of carbohydrates in metabolic disease was clearly understood—and metabolic disease was very rare.
I grew up eating lots of animal meat: pork, bacon, beef, eggs, poultry—including duck and geese—and organ meats, including liver, kidneys, bone marrow, heart, gizzards, pork ears, snouts, hoof, chicken feet, even chicken blood, pork and beef blood in sausages, such as blood sausage—still sold in many places—cooked in pork lard, duck fat butter, or beef tallow, and lots of fatty fish. We also ate a lot of dairy, including milk and cheeses plus all other dairy forms. We had various dairy and cultured milks as well. Of course, we drank milk that could be placed in the window for a day and by next day it was kefir without any added culture and without rotting. Our staples were potatoes, beans, rice, onions, and apples that lasted through February in cold storage. Other fruits and vegetables were all only seasonal, lasting a very short time.
We didn’t have processed foods and processed oils of any kind. While some canned foods and sweetened drinks certainly existed, those were seldom consumed. There was no such as daily dessert. If I was a good girl, maybe once a month I was taken to special pastry places and I could pick one dessert. If you think my family was poor and hence I was eating this way, you are wrong. I was a privileged child. I spent several of my childhood summers in the South of France eating more seafood, but basically the same exact diet. The European diet, when I grew up, was a very cholesterol rich fat-heavy low carbohydrate diet.
It is important to note that while cholesterol levels have been consistently dropping over the past several decades(2)—as a result of the recommended SAD diet full of vegetable oils—the rates of cardiovascular and metabolic diseases have been increasing over the same period, indicating a possible inverse relationship. This is promptly ignored by medicine and there is a continual push toward the consumption of lower cholesterol foods, such as whole grains, fruits and vegetables, and vegetable oils. This, in spite of several studies showing the above mentioned inverse relationship, suggesting that higher cholesterol extends healthy lifespan(3,4). The reason I mention cholesterol is because a reduced carbohydrate diet, such as the one I grew up on, is necessarily a heavy saturated fat and cholesterol diet.
Yet, during those years in Europe, metabolic diseases (such as non-alcoholic fatty liver, cardiovascular disease (CVD), stroke, type 2 diabetes, etc.,) were rare. This article shows the confusion. In it, they discuss the rates of CVD, which was very low in France at the time, to be caused by a “lag”. The assumption being that the heavy saturated fat-filled foods will catch up with the French and they will eventually develop CVD. Interestingly, the French ate heavy saturated fat for centuries before this study, so the catching up is a silly theory aiming to explain the French Paradox. And the catching up is still going on without any success—though now that American junk food is available to the French, it may be only a matter of time.
Ketosis
When one consumes a low carbohydrate high fat diet, even with high protein and some beans time to time, the person will be in a state of ketosis. In ketosis, the body can use both glucose and fat (both consumed and stored fat) as its fuel. Fat is converted to ketones, or β-Hydroxybutyrate (BHB). This state is reached by diets rich in animal fats, medium amounts of protein, and little or no carbohydrates. Rather than hindering health, ketosis supports and protects it (5), as it can be seen in the treatment of epilepsy(6). Ketosis is the basic human metabolic process. This is further discussed later.
Carbohydrates Versus Fats
When some time ago I bumped into the book Metabolic regulation: A Human Perspective by Keith N. Frayn (3rd edition), in chapter 2.1 and 2.2 I came to two very unusual sections that made me jump up.
The chapter section states the following:
“…fatty acids are usually a preferred fuel (over glucose) for skeletal muscle… Fatty acid release is very effectively switched off by insulin, so muscles no longer have the option of using fatty acids… The characteristics of individual cells or tissues ‘set the scene’ for metabolic regulation. For instance, the metabolic characteristics of the liver mean that it will inevitably be able to take up excess glucose from plasma, whereas other tissues cannot adjust their rates of utilization so readily… The brain, in contrast, has a pathway for utilizing glucose at a rate that is relatively constant whatever the utilizing glucose concentration, a very reasonable adaptation since we would not want to be super-intelligent only after eating carbohydrate, and intellectually challenged between meals.”
I was surprised. In all literature that advises healthy nutrition, we are told to consume a ton of carbohydrates. The USDA Dietary Guidelines recommend My Plate (what used to be the food pyramid, see the history of the USDA guidelines here), which is mostly carbohydrates, with a little bit of meat or fish, eggs, dairy, and some oil on top. Basically most of the diet—over 60 percent—is supposed to come from carbohydrates, such as whole grains, fresh fruits, vegetables, nuts, and seeds. Those are all carbs. The paragraph from the book was intriguing to me, because it tells us that we don’t need to eat carbs, contrary to USDA dietary recommendations.
Skeletal muscles actually prefer to use fat rather than glucose! We have a very carbohydrate-centric view of nutrition today, much more so than when I grew up, yet our muscles and some other organs too, such as the heart(7,8), actually prefer fat as fuel and not glucose! Why are we eating so many carbohydrates?
The Fuels of Our Body
Few professionals, even within the field of nutrition, realize that glucose is not our primary fuel and ketones are not our backup fuel. The human body has no primary or backup fuel: it has three fuels. Some of these fuels are toxic if they stay in the blood too long in larger amounts than needed, and so the body must remove them fast. I presume that the urgency for glucose use—meaning the urgency for the removal of glucose from the blood—is misleading and makes people think that if the body switches to using glucose the moment it is provided, it must be its primary fuel; but this is incorrect assumption. This suggests that the first task that has to be done is the preferred task, but this is seldom the case. For example, assume you trip on your way to a dinner party, hit your head into the cement, and now see double. Although your urgent task now is to head to emergency to see if you received a concussion or other serious damage, the emergency visit is not your preferred task. It just suddenly became a priority you need to tend to immediately before you join the dinner party.
It is true that when we eat carbohydrates, the body must stop everything and remove the excess glucose from the blood. The maximum comfort level for glucose in the blood is 99 mg/dL (5.5 mmol/L) and if we eat carbohydrates in such amounts that this is exceeded, it is literally an emergency and the body must remove the excess glucose. For reference, 99 mg/dL is one teaspoon of glucose in the entire 5 liters of blood. Extra glucose in the blood is toxic. However, having to remove glucose immediately does not make it into the primary fuel.
The three fuels our body can use are: alcohol, providing 7 kcal per gram, glucose, providing 4 kcal per gram, and fat, providing 9 kcal per gram. While alcohol is a viable fuel for the human body, it creates many adverse effects, causing damage, so it is not recommended to be used as fuel, though alcoholics often use it as such. Given that alcohol is the most dangerous of all the fuels(9), if our body is provided the three fuels simultaneously, alcohol will be burned first. Yet we don’t ever assume that alcohol is our primary fuel.
How the Body Prioritizes Fuels
Priority can be assigned for many reasons. One can give priority to something preferred, but if this means that something harmful has to wait to be removed, there is a risk of disease. If this was the method our body chose for prioritization, we may not have remained alive long enough to become who we are today. One can prioritize by the amount of energy each fuel gives, using up first the one that gives the most energy, and saving the rest for later. But, again, if the rest causes damage while waiting to be used, then this has to be avoided. One can also prioritize based on the removal of toxic fuel first and save the least toxic fuel to be used last.
If our body prioritizes based on preventing damage by burning the fuel in order of toxicity, then the order would be:
- Alcohol
- Glucose
- Fat
If priority would be given to those fuels that provide the most energy, the order would be:
- Fat
- Alcohol
- Glucose
If the priority is based on the USDA dietary guidelines, then the order would be (alcohol as fuel is usually not mentioned anywhere):
- Glucose
- Fat
What we actually see happening is that the body burns fuel in the order of which it causes the most damage in the blood. The most dangerous fuel in the blood is alcohol. Its side effects can even be fatal, so clearing that from the body is necessarily task #1.
The urgency with which we must respond to the situation is dependent upon its outcome.
Glucose is the second most dangerous fuel in the human body after alcohol. Fructose, a sugar that is part of table sugar, honey, and most fruits, turns into ethanol (an alcohol) causing damage, and glucose—referred to as blood sugar—is toxic to our nerves, may cause eye damage and type 2 diabetes, and cardiovascular disease (including stroke) as well.
By contrast, fat is a safe fuel to the point that it is usually stored in our body—something many of us wish to have less of. It is not a toxic substance and at 9 kcal per gram, it provides the most energy. Alcohol inhibits the burning of glucose and fats, making it the mandatory first fuel to burn. So the actual order of fuel priority is:
- Alcohol
- Glucose
- Fat
So why was I so surprised reading that some organs prefer to use fat for fuel? We read and hear so much about carbohydrates as the most important fuel, the kinds of carbohydrates we should be eating, and how much. We can learn very little about the other important fuels: alcohol and fats. Yet, as the surprising paragraph suggests above, often the other fuels are more important. In particular, if we look at the human lifespan, other fuel needs become stunningly obvious. I think we have forgotten that babies are born in ketosis and their primary fuel is ketones.
Human Fuel from Conception
Indeed, babies are born in ketosis(10) and mother’s milk is low in carbohydrate and high in fat (LCHF), which keeps the newborn in ketosis all through nursing. Breast milk contains more glucose across time, as the child matures. At full maturation (about one month), its nutritional content per cup (8 oz) is 10.8 gr fat, 2.53 gr protein, 16.9 gr carbohydrates (in the form of lactose) and total energy of 174.92 kcal. It also contains 87.5 gr water. Subtracting the water and looking at the macronutrient ratios only, this glass of mature nursing milk is 55.57% fat, 5.79% protein, and 38.65% carbohydrates (in lactose, so not free sugar). In terms of fatty acid composition: 4.942 gr saturated fat, 4.079 gr monounsaturated fat, and 1.223 gr polyunsaturated fat, which in percentages: 48.24% saturated fat, 39.82% monounsaturated fat, and 11.94% polyunsaturated fat. One must agree that babies are not fed poison by their mothers and that Nature didn’t provide toxic nursing milk such. In fact, we can see that babies grow very rapidly while nursing milk and we know from studies that babies who are nursed, have a better chance for survival, grow healthier, faster, and their brain develops better (see here and here).
As babies grow, they retain metabolic flexibility, meaning they stay in ketosis for periods time, which changes by age and how often they are fed, and they do enter the carbohydrate metabolic process as they eat(10-12).
The below figure is very telling. On the vertical axis you find β-hydroxybutyrate [BHB], which is the level of ketones measured in blood, and on the horizontal axis, time passing in hours and days between feeding times. The graph inside contains people of all age groups and both genders. Officially, a fed person (with carbohydrate containing food) has zero amount of BHB in her/his blood. As time passes, and if the person fasts for a blood test or a medical procedure, slowly BHB increases in the blood. The clinically accepted level of BHB in the blood that is not considered ketosis is 0.3 mmol/L, which can easily be reached by healthy individuals as a result of such fasting. Anything above 0.3 mmol/L and chronically maintained 0.3 mmol/L means the person is in ketosis.
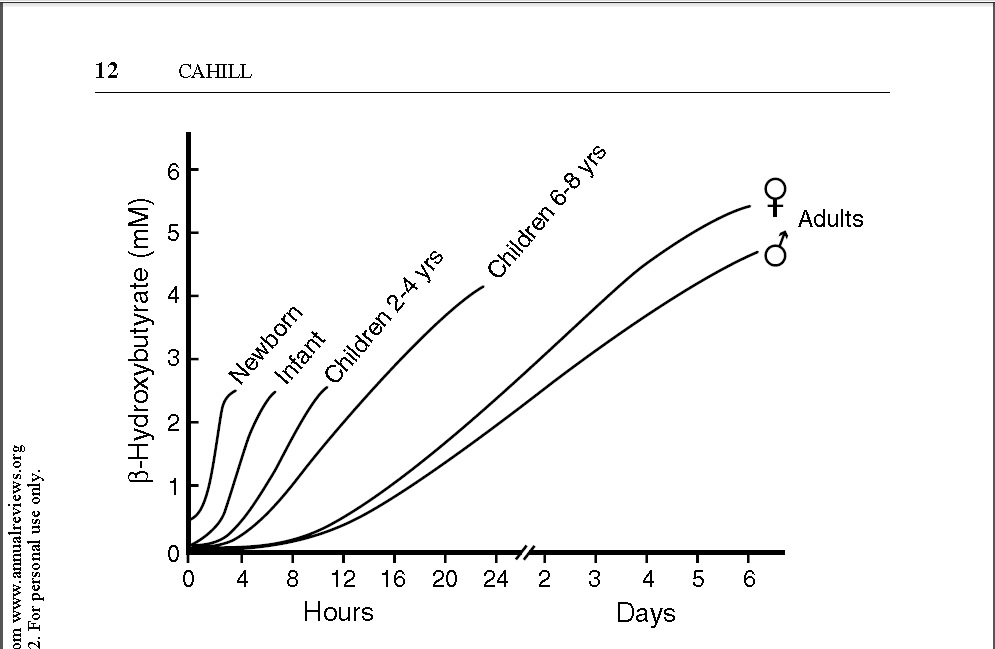
From Annu. Rev. Nutr. 2006. 26:1–22; doi: 10.1146/annurev.nutr.26.061505.111258
Figure 1. George F. Cahill Jr. showing time passing without food and ketosis level by age and gender
Note that babies are born with 0.5 mmol/L or higher level of BHB and remain in ketosis until they are fed, which immediately after birth cannot happen since the mother has no milk yet—this means the baby remains in ketosis until the time comes that milk is released by the breast of the mom. It is suggested that the baby is in ketosis because it is not being fed(10), meaning starvation, but this is questionable, since babies remain in ketosis even after being fed—more on this later. The human brain uses 20% of the energy the body generates. In the case of infants, the need for energy arises very quickly, as shown in Figure 1, approximately in 20 minutes. There are other factors as well, such as the brain is over 80% fat and cholesterol(13), with the cholesterol alone representing 20-25% of the total cholesterol of the body (here).
Thus ketosis, in one scenario, is a state into which our metabolism reverts to when food is not immediately available on demand (starvation). On the other hand, studies on the fetus in utero show that the fetus is in ketosis even though it is never under nutritional duress(14,15) and there are ketones in the placenta(16) as well. Therefore, it is very difficult to suggest that ketones are a backup fuel used only in starvation if the fetus is in ketosis time to time even without starvation. Clearly, being in ketosis provides some benefits that are not possible to achieve using the glucose metabolic process. I venture to suggest that the ketogenic and the glucogenic metabolic processes have distinct functions, each to benefit us on its own way.
Concluding Thoughts
To conclude the importance of ketosis, let me offer some anecdotal evidence. In the Facebook migraine groups I manage (see here and here), all migraineurs are asked to run a special blood glucose/blood ketone test that starts with fasting and premeal tests and continues for 5 hours postprandial. There are many children with migraines whose parents are in the groups—the children are from ages 2-18, so for them parental help is required. Thus, over time, I have had the opportunity to evaluate the 5-hour blood test results of children of all ages—I think the youngest was 5 years old and the oldest 16, so far. I have yet to see a blood ketone test of a child anywhere in this age group that is not showing ketosis both before and after a meal—even if the meal has fruits and dairy in it.
I suppose ignorance is bliss. Few doctors or researchers have the same opportunity I have in being able to measure the blood ketones of various ages of children for five hours postprandial plus fasting and premeal measures, therefore, most don’t realize just how much our kids are in ketosis.
Thus, while today in most countries around the world any type of food is just a short walk/drive away 24/7, and we need not experience hunger and starvation, our children are still in ketosis 24/7. Shouldn’t that tell us something about the importance of ketosis?
References
- Dawkins, M. Carbohydrates and Adiposity. British medical journal 1, 719-720, doi:10.1136/bmj.1.5385.719 (1964).
- Farzadfar, F. et al. National, regional, and global trends in serum total cholesterol since 1980: systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3.0 million participants. The Lancet 377, 578-586, doi:10.1016/S0140-6736(10)62038-7 (2011).
- Ravnskov, U. High cholesterol may protect against infections and atherosclerosis. QJM: An International Journal of Medicine 96, 927-934, doi:10.1093/qjmed/hcg150 (2003).
- Kaysen, G. A. et al. Lipid levels are inversely associated with infectious and all-cause mortality: international MONDO study results. Journal of lipid research 59, 1519-1528, doi:10.1194/jlr.P084277 (2018).
- DuBroff, R. & de Lorgeril, M. Fat or fiction: the diet-heart hypothesis. BMJ Evidence-Based Medicine, bmjebm-2019-111180, doi:10.1136/bmjebm-2019-111180 (2019).
- Berghoff, S. A. et al. Dietary cholesterol promotes repair of demyelinated lesions in the adult brain. Nature communications 8, 14241-14241, doi:10.1038/ncomms14241 (2017).
- Park, T.S., Yamashita, H., Blaner, W. S. & Goldberg, I. J. Lipids in the heart: a source of fuel and a source of toxins. Current Opinion in Lipidology 18, 277-282, doi:10.1097/MOL.0b013e32814a57db (2007).
- Noh, H.-L., Yamashita, H. & Goldberg, I. J. Cardiac Metabolism and Mechanics are Altered by Genetic Loss of Lipoprotein Triglyceride Lipolysis. Cardiovascular Drugs and Therapy 20, 441-444, doi:10.1007/s10557-006-0633-1 (2006).
- Van de Wiel, A. Diabetes mellitus and alcohol. Diabetes/Metabolism Research and Reviews 20, 263-267, doi:10.1002/dmrr.492 (2004).
- Cahill, G. F. Starvation in man. N Engl J Med 282, doi:10.1056/nejm197003052821026 (1970).
- Storlien, L., Oakes, N. D. & Kelley, D. E. Metabolic flexibility. Proceedings of the Nutrition Society 63, 363-368, doi:10.1079/PNS2004349 (2007).
- George F. Cahill, J. Fuel Metabolism in Starvation. Annual Review of Nutrition 26, 1-22, doi:10.1146/annurev.nutr.26.061505.111258 (2006).
- Chang, C. K., DS; Chen, JY;. Essential fatty acids and human brain. Acta Neurologica Taiwanica 18, 10 (2009).
- Herrera, E. & Amusquivar, E. Lipid metabolism in the fetus and the newborn. Diabetes/Metabolism Research and Reviews 16, 202-210, doi:doi:10.1002/1520-7560(200005/06)16:3<202::AID-DMRR116>3.0.CO;2-# (2000).
- Herrera, E. Lipid metabolism in pregnancy and its consequences in the fetus and newborn. Endocrine 19, 43-55, doi:10.1385/endo:19:1:43 (2002).
- Orczyk-Pawilowicz, M. et al. Metabolomics of Human Amniotic Fluid and Maternal Plasma during Normal Pregnancy. PloS one 11, e0152740-e0152740, doi:10.1371/journal.pone.0152740 (2016).
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image credit: Creative Commons Attribution (CC BY 4.0) terms and conditions https://creativecommons.org/licenses/by/4.0 Baby. Credit: Bill McConkey. CC BY















When the milk starts to flow varies by mom and her body, but regardless when it starts, it is always very high in fat with “mature nursing milk is 55.57% fat, 5.79% protein, and 38.65% carbohydrates (in lactose, so not free sugar)”
This is not the answer you get when you google what’s in breast milk. I’ve tried to use your break down in arguments but Google says differently. How do I explain this to people?
Thank you
Ted
Dear Ted,
The only information people can get about mother’s milk is from the USDA database, which is only for mature human milk: https://fdc.nal.usda.gov/fdc-app.html#/food-details/171279/nutrients and according to this, mature human milk has 39.42% fat, 4.12% protein, and 27.56% carbs–this is percent by Calories. The percent by weight is 55% fat, 6% protein, and 39% carbs. These numbers align with the numbers you gave, so you are listing the percentage by weight.
Please be cognizant of the differences in percentage by weight vs by Calories. So this may be one of the discrepancies you found.
I have no idea what answer one gets from using a Google search. I wouldn’t follow Google on something this specific. For nutrition information, follow the USDA database.
Angela
If a child goes in and out of ketosis just due to how they eat, could they possibly get that bad breath smell, acetone like? Thanks.
Dear Stacy,
It isn’t likely that kids get bad breath from ketosis because bad breath in ketosis is actually associated with not being able to use ketones as fuel, and kids are very well adapted, unless there is a pathological reason for such. Let me explain.
There are 3 ketone bodies made by our liver:
1) Acetone–what you smell; acetone is spontaneously created from acetoacetate
2) Acetoacetate–what is in urine. A form of acetoacetic acid, is the base that can be converted by the liver into BHB. The acetoacetate that is not converted into BHB is urinated out.
3) Beta-Hydroxy-Butyrate (BHB)–what we burn as fuel that we refer to–in terms of metabolism–as ketones. So “ketosis” refers to the “burning of BHB” but not the other ketone bodies.
What you smell on people who aren’t efficient in ketosis is the acetone in the breath, because they aren’t able to burn ketones, and this can happen for a variety of reasons. For example, insulin release prevents the burning of ketones and so every time our body releases insulin for tasting of food, thinking of food, smelling of food, or looking at food, we experience cephalic insulin release. Think of this as a Pavlovian reaction which prepares our body for the arrival of food. Eating food and burning ketones don’t typically coexist since the burning of ketones is reserved for the times of fasting.
Another reason for such odor would be the inability to burn ketones and the inability to get rid of glucose in the blood–in this case you will find both high blood glucose and high blood ketones. This would be in the case when the pancreas fails and insulin cannot be produced by the body anymore. This is ketoacidosis. This is typically end-stage type 2 diabetes and also type 1 diabetes.
And there is one more important point: in ketosis basically we place our brain into the state of ketosis and not the rest of our body. While some of our other organs can also burn ketones, most of our organs usually burn fat, rather than ketones, for fuel. The fat we usually burn are non-esterified free fatty acids (triglycerides). Ketone BHB is a fatty acid but it is a much smaller molecule and can cross the blood brain barrier, where triglycerides cannot. So our muscles, heart, liver, etc., all usually burn triglycerides for energy though they all can burn glucose as well, and most can also burn ketones except our liver. The liver cannot burn ketones, only free fatty acid and glucose. And our red blood cells and eyes can only burn glucose becuase they lack mitochondria.
With all this background, you can see that the state of “ketosis” (when not pathological) is really only the brain using ketones instead of glucose. In addition, children are very much adapted to ketosis since they were in ketosis in the womb, were born in ketosis, remain in ketosis 100% prior to first nursing, and fall back into ketosis within minutes after nursing. So children are in and out of ketosis all through infanthood and they don’t have “keto breath” then. Or at least they shouldn’t!
If you smell keto breath on your child, I recommend you have a pediatrician examine the child for type 1 diabetes. Type 1 diabetes is a state in which glucose isn’t able to be removed from the blood by insulin because the child has no insulin. While those organs that don’t use insulin do well, such as the brain, which doesn’t have insulin receptors and glucose uses sodium transporters to get into the neurons, muscle cells have insulin receptors and insulin must be used to carry glucose into muscle cells. If there is no insulin, ketone bodies build up to a very large level and the breath as well as the body will pick up an acetone-like odor. This represents that the blood pH is dropping, meaning it is getting more acidic than it should be.
If your child has acetone body or breath odor, you need to have them tested right away. Type 1 diabetes is often misdiagnosed for type 2 diabetes, because in both cases the blood glucose level is very high. However, the high blood glucose is just a symptom and is not a sufficient evaluation. Please be sure to have your child’s insulin, c-peptide, lipase, diabetes antibodies, oral glucose tolerance test with both glucose and insulin, glucose in the urine, protein in the urine, ketone in the urine all tested to rule out type 1 diabetes.
Good luck to you and let us know how things turn out!
Angela
I had a child in ketosis (according to urine tests) despite eating a high-carb diet, and it was caused by thiamine deficiency. After supplementing thiamine along with other B vitamins, testing showed he was no longer in ketosis. (His labwork suggested various indicators of likely thiamine deficiency, but it was the being in ketosis which was the biggest red flag which made us start with thiamine.)
I don’t think it’s any great stretch of the imagination to believe that kids with migraines are among those more likely to have sub-optimal B1 status. I don’t think the prevalence of ketosis in kids with migraines necessarily tells you about the importance of ketosis – it could just show the prevalence of disordered metabolism in kids with migraines.
Dear Kt,
If you read the article, I placed lots of citations that you can follow up on. It is not an article about kids in migraine: all kids are in ketosis. All kids are born in ketosis and remain in ketosis trough nursing. And, provided that instead of formula they get real food, babies remain in ketosis through age 10. This has been studied and documented by others–this is well known. I cited some articles in my blog but there are many more.
Migraine suffering kids are not any more likely to be in ketosis than other kids. Migraineurs are also not more likely to suffer from B1 (thiamine) deficiency than other people.
B1 is a carbohydrate management vitamin and if you child has B1 deficiency and cannot efficiently burn carbohydrates as a result, that’s a problem.
Mind you, people–including kids–who are efficiently in ketosis, don’t show ketones in their urine. Ketones in the urine would be ketones not used–the body eliminated them. This doesn’t happen with people who are in efficient ketosis. For example, I have been in ketosis for 5 years and my urine test has yet to catch it once, but the blood test always catches it. The only valid measure of true and healthy ketosis is via the measuring of it in the blood.
This is very similar to glucose in the urine: it will not be there if one is burning glucose efficiently. Glucose only spills into the urine if it is not metabolized properly, which happens in T1D and T2D. A metabolically healthy individual will not have glucose in his/her urine. This is exactly the same with ketones.
Best wishes,
Angela
In the article you said that a baby cannot get out of ketosis because there is no milk and that they will remain in ketosis until the mother’s milk comes in, but mother’s have something called colostrum in their breasts at borth and that is what babies eat at first. I do not know the nutritional content, but I do know that it is very high in fat as it has an extremely oily consistency. I just wanted to share that with you in case you don’t already know.
Thanks Nicole, correct. The mom has colostrum, which is very high in fat, further supporting the baby’s ketosis. There is no milk in colostrum.
When the milk starts to flow varies by mom and her body, but regardless when it starts, it is always very high in fat with “mature nursing milk is 55.57% fat, 5.79% protein, and 38.65% carbohydrates (in lactose, so not free sugar)” when it fully matures. So it remains to have extremely high fat content, keeping the baby in ketosis. 🙂
Thanks for your comments,
Angela