Vitamin A is a nutritional term for a group of compounds with specific structures, of which the principal vitamer is called Retinol. Vitamin A derivatives (Retinol, Retinoic Acid, Retinal) are required for several functions involving immune, metabolic, embryonic development, and transduction of light signals in the eyes. Deficiency of this important vitamin is the commonest preventable cause of blindness in the world. While the latter may be end result of a severe chronic deficiency, like many other nutrients, the body will exhibit different symptoms based on the spectrum (or level) of deficiency. Also like other nutrients vitamin A status is affected by, and can affect, multiple pathways. For example, inadequate zinc intake will cause a functional vitamin A deficiency, and when vitamin A is low, whether by functional or frank deficiency, multiple metabolic pathways will be downregulated.
Vitamin A Status Is Dependent Upon Zinc
Vitamin A and zinc are interrelated. In the setting of low zinc, Vitamin A cannot circulate in the body. This is because Vitamin A requires Retinol Binding Protein (RBP) for circulation, and the production of (RBP) is in turn dependent on sufficient levels of zinc. This means that even if the liver has sufficient stores of Vitamin A, a deficiency of zinc will cause functional hypovitaminosis A due to inability to utilize liver Vitamin A stores [Tietz Textbook of Laboratory Medicine, 7th, pg 2186]. In fact, studies have shown that simultaneous zinc and Vitamin A supplementation is clinically more effective than supplementing with these compounds alone. Similarly, someone who has an ongoing/chronic inflammation can also have reduced RBP, and therefore functional hypovitaminosis A.
Pathways Dependent Upon Vitamin A
Thyroid Function
Vitamin A compounds exert their effects through multiple mechanisms, including at the genomic level. For example, the active thyroid hormone, T3, cannot drive its effects on the genome efficiently without combining with retinoid X receptors (RXR) – RXR is activated by Vitamin A derivatives. Therefore, functional or cellular hypothyroidism can be mediated by a vitamin A deficiency. Vitamin A has additional positive effects on thyroid hormone homeostasis, including a role in the production of thyroid hormones (Figure 1). For example, deficiency of vitamin A can impair iodine uptake in the thyroid – an essential step for the production of thyroid hormones T4 and T3. Similarly, reduced levels of Vitamin A cause lowered tissue conversion and uptake of T3, including in muscle tissue. Interestingly, the same protein required for Vitamin A transport (RBP), is also involved in regulating (by physically binding) the function of the thyroid hormone transporting protein Transthyretin (TTR). In this case, the affinity of thyroid hormone to TTR becomes lower in absence of RBP.
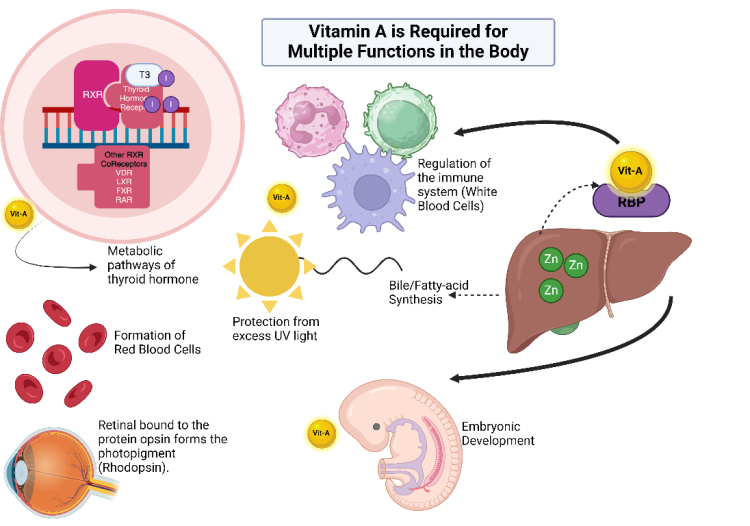
Liver Function
The liver and other cells express receptors named Liver X Receptor (LXR). Just like the thyroid hormone receptor and vitamin D receptor, LXR requires binding with RXR (Vitamin A dependent) to propagate its signals. What happens when LXR and RXR activate gene signals? Several important enzymes and proteins are produced which include:
- Acetyl-CoA carboxylase. This biotin-dependent enzyme sits atop fatty acid synthesis pathway and is downregulated when vitamin A concentrations are low resulting in reduced ability to make cell structures (membranes), energy, and molecules important for cell communication.
- Cytochrome P450 CYP7A. This enzyme is important for converting sterols (i.e. cholesterol) to bile. When vitamin A is low, this will potentially cause reduced absorption of fat-soluble substances such as vitamin K, D, and A.
- Cholesterol transport proteins like apoCI, apoCII, apoD, and apoE are affected by low vitamin A. Abnormalities in these enzyme can cause abnormalities in lipid metabolism, including the metabolism of HDL and VLDL.
- GLUT4. GLUT4 is a muscle and fat tissue transporter of glucose. GLUT4 is regulated by insulin, and its expression is further mediated by Vitamin A metabolites in the DNA through the RXR receptor. Therefore when vitamin A is low, insulin-mediated signals may not work optimally.
Other receptors that need RXR to function include the Retinoic Acid Receptor (RAR), and Farnesoid X Receptor (FXR).
Sun Exposure and Vitamin A Reserves
Lifestyle habits can play a role in depleting Vitamin A. For example, excessive sunlight can deplete Vitamin A reserves. This is because retinyl esters, also concentrate in the epidermis (outer layer of skin), and is able to absorb Ultra Violet light (300-350 nanometers). Here Vitamin A metabolites can function as a filter when the body is exposed to too much sunlight by absorbing excess energy from the sun. Therefore, during a Vitamin A deficiency there would be a higher probability of increased UV-induced damage to DNA, and flavins (Riboflavin/Vitamin-B2). Therefore in terms of electromagnetic radiation, the body works in concert where retinyl esters protect the skin while the body is absorbing beneficial red/infrared light in conjunction with production of Vitamin D via UVB energy.
Development of the Embryo
The retinoic acid signaling pathway is essential for cell differentiation (making different cell types) and overall development of the human embryo. This Vitamin A-based signaling is tightly regulated by the cells of the embryo, and indeed too little or too much of Vitamin A signals can cause problems like congenital malformations. The reason why Vitamin A is important is because its derivates need to bind to two receptors, RAR and RXR, that then coordinate the production of developmental gene signals required for proper embryogenesis.
Iron and Copper Homeostasis
Anemia can be caused by low Vitamin A reserves, although the mechanism behind this relationship is not well understood. The anemia is likely mediated in-part through the mechanism of induction of ceruloplasmin (copper containing protein) by retinoic acid. In this case, less retinoic acid (or Vitamin A) causes lower available copper to tissues for blood cell formation. To read more about copper, anemia, and thyroid hormones see this article.
The above are some of the many enzymes and pathways co-regulated by Vitamin A metabolites. We can see from this list how chronic Vitamin A deficiency can affect thyroid function, fatty nutrient absorption, formation of important cellular components, Vitamin D signaling, iron and copper homeostasis, and eventually ATP production.
How Can We Determine if Vitamin A Is Low or Functionally Deficient?
Current methods for evaluating status of Vitamin A via serum analysis, though convenient, do not provide an ideal assessment of hypovitaminosis A (i.e. vitamin A deficiency). The reason is because Vitamin A is mostly stored in the liver, and serum levels may not reflect deficiency until the levels of vitamin A become critically low (about 20 micrograms per gram of liver). In other words, serum Vitamin A concentrations can stay somewhat constant even when the liver stores vacillate significantly. Other tissues in the body are able to concentrate Vitamin A to a lesser extent, such as the skin.
Since serum Vitamin A levels may not always be clinically accurate, the following should be evaluated with or without serum Vitamin A levels:
- Clinical symptoms. Classical symptoms include: changes in eye and skin, night blindness, bitot spots. Other not so well recognized symptoms include leaky gut, immune deficiency, hair loss especially in head but also in the arms for men.
- Functional Vitamin A Deficiency. Check levels of intracellular zinc, if the patient is showing deficiency symptoms despite evidence of a Vitamin A rich diet. Supplementing with Vitamin A without correcting a zinc deficiency may cause more problems.
- Macronutrient intake. Assess the patient’s macronutrient intake, especially protein. If total protein is low, then chances are that the RBP protein will also be suboptimal
- Vitamin A intake. Determine if the patient’s intake of Vitamin A rich foods is adequate. Note that celiac disease, pancreatitis, low stomach acid, or other disorders causing decreased absorption of fatty nutrients (or protein) can predispose individuals to lower vitamin A intake and/or lowered bioavailability. Zinc levels can also be affected by these conditions.
- Zinc intake or status. Zinc is an essential mineral and must be obtained from dietary sources. Deficiency of zinc not only compromises the utilization of Vitamin A from the liver, but will lead to more cellular dysfunction. The latter includes, reduced stomach acid, reduced activity of zinc-dependent enzymes, and lowered immunity. Here, we can see that reduced zinc levels exacerbates the problem of total nutrient intake, leading to worse outcomes – such as Vitamin A deficiency. Zinc is best evaluated using intracellular assays (Zinc, RBC). Those proven to be lower in zinc should abstain from vitamin A supplementation until zinc levels are corrected. The RDA for zinc is approximately 8-15 mg per day. Those showing lowered intracellular zinc levels, with their physician’s guidance, should intake at least 60 mg per day for 4 weeks and then re-evaluate. For more information regarding zinc deficiency and other associated disorders, we refer the reader to the following articles:
- Chronic inflammation. Chronic inflammatory illnesses will reduce levels of RBP. To determine if the patient has a functional Vitamin A deficiency due to nutritional or inflammatory reasons (or both) then CRP, or other inflammatory markers, should be added to the diagnostic test repertoire.
Is Vitamin A Toxic?
As mentioned above, Vitamin A compounds are essential for proper function of cells and hormone producing glands. However, like every nutrient or essential substance (e.g. as simple as water), excess can produce problems. Since Vitamin A is stored mostly in the liver, there is the potential for hepato- and systemic toxicity which is estimated to be when levels reach approximately 3000 micrograms per gram of tissue. In supplemental terms, toxicity can occur when ingesting more than 30000 micrograms per day (100000 IU) for months to years. In other evaluations, taking Vitamin A supplements >10 times the RDA (700-900 micrograms) for more than 3 months may cause hypervitaminosis A to those susceptible.
Although toxicity levels vary between studies, the consensus is that it will take large doses for long periods of time for toxicity symptoms to appear. In this case, plasma level of Vitamin A can be reflective of toxicity (>140 micrograms/dL). Symptoms of hypervitaminosis A are generally reversible upon ceasing of Vitamin A supplementation. Asserting that one is Vitamin A toxic without direct experimental (tissue biopsy), biochemical (very high plasma levels, high liver enzymes), or strong clinical evidence (amalgamation of toxicity symptoms post supplementation), is simply misleading. Given the clear dependency of Vitamin A on zinc, it is my opinion that potential toxicity by Vitamin A is likely potentiated by a zinc deficiency which stifles transport of Vitamin A out of the liver. Overall, like every vitamin or supplement, a balanced approach should be taken with this essential vitamin.
Vitamin A and Its Regulators Are Essential to Cellular Metabolism
Vitamin A is a group of essential compounds required for proper cell and organ function. Deficiency can cause a host of classical and non-classical symptoms. Vitamin A, through binding to its receptors RXR and RAR, drives several important functions within the DNA including thyroid hormone receptor activation, genes central to cell differentiation and development of the embryo. As discussed above, thyroid metabolism is dependent on Vitamin A even beyond the DNA gene expression levels. Without sufficient Vitamin A the body not just becomes less efficient in making thyroid hormones, but also becomes less capable of converting thyroid hormones into active form T3.
Importantly, without zinc, functional deficiency of Vitamin A will occur. This is because cells of the body requires optimal levels of zinc in order to properly regulate and use Vitamin A. Testing for Vitamin A via blood/plasma can be helpful but does not necessarily imply optimal levels of the Vitamin A in tissues. The liver may have enough stored unusable Vitamin A (due to low zinc), or it may be that total stores have been depleted. Additionally, individuals who are reaping the benefits of sunlight should consider checking their Vitamin A intake, as it is a protective mechanism for the skin under UV light – but at the expense of its depletion. Overall, it is best to evaluate symptoms, dietary patterns, in conjunction with blood work.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Photo by Bradyn Trollip on Unsplash.
This article was published originally on November 19, 2024.















