At age 23, I woke up from an ovarian surgery to the comment, “It’s not cancer, but you have moderate endometriosis. If I were you, I’d get pregnant as soon as possible.” Having only been married for a year, and not yet stable in our financial situation, we just laughed, not really understanding what the doctor meant. And I decided to go right back onto the birth control pill.
Five years later, at age 27, on our anniversary trip we decided it was the perfect time to get off of the pill and try getting pregnant. I remember throwing the packs of pills away, excited for the future to come. Little did I know that would start a whole snowball effect that would ultimately take my health and my fertility.
A year later, I was starting to have odd symptoms. I began having massive acid reflux that was burning my voice box severely. I was quickly started on a Proton Pump Inhibitor. I was never told that it should’ve been a limited time treatment, so I continued taking them. Pretty soon, I started having issues with my menstrual cycles. I noticed that the bleeding was getting heavier and heavier and the pain was increasingly getting worse. It never occurred to me that any of that was in any way abnormal. I just figured it was part of being a woman, and I needed to suck it up.
Severe Menstrual Bleeding and Panic Attacks: Unrecognized B12 and Iron Deficiencies
On October 6th, 2006, I woke up to severe bleeding and panic attacks. My husband rushed me to the doctor where I was diagnosed with severe iron deficiency. My ferritin (stored iron) was incredibly low; almost non-existent. I was sent home with iron pills and instructions to take them once a day. Quickly my health began to decline, and many mornings I would wake up in a sweat and a full panic. I knew something was wrong but all of the tests kept coming back normal. Two years later, when my doctor retired, I received my records and immediately noticed my B12 was also extremely deficient, so I started supplementing B-vitamins on my own. I slowly gained a little energy back, and was able to function semi-normally for a while, however, I still had this underlying anxiety that I couldn’t shake.
Back on Birth Control and Still No Relief
My next option was to go back onto birth control and see if it would control the increasingly heavy and painful menstrual cycles I was having. Unfortunately now, any pill I tried, my body and my anxiety went into a major downward spiral, leading me to quickly come off of any hormone pills. By this time, I was seeing multiple doctors. My bleeding had become very uncontrollable, and I was soon diagnosed with a fibroid. I considered Uterine Artery Embolization, but at that time my fear of losing my fertility was too prominent to go ahead and proceed with the surgery. I continued to increase my iron intake, and after lots of research, I learned a regimen that seemed to work for me. Regular lab testing showed me constantly dropping in iron and blood levels, and then recovering some, and then dropping severely again when my cycle came around. Eventually my cycles got so intense that I was having to use incontinence overnight pads instead of the regular menstrual pads. It was a nightmare. I began to get more and more bed ridden and ended up having to bring in outside help to just help me get through my day, while my husband went to work to provide for our home and my medical needs.
Dropping Blood Pressure, Skyrocketing Heart Rate: I Was Close to Dying
The day after Thanksgiving 2013, which my husband and I had spent alone due to my inability to leave the house, found me unable to get up without almost passing out. My blood pressure was incredibly low and my heart rate was more than 160 beats per minute. I brushed it off as anxiety, but my neighbor who was a paramedic’s wife came by and took one look at me and told me, “Get to the hospital RIGHT NOW!!!” My husband loaded me up into the car and we went. I wasn’t a stranger to the emergency room, but was usually sent home with the comment “take more iron” or “go see your doctor” (which I was, but evidently I wasn’t getting the monitoring or treatment I needed).
So I sat in a wheelchair in the waiting room, waiting for my turn to be called and suddenly two nurses ran out of the doors and headed for me. I looked at my mom who had joined us at the emergency room, knowing instantly this couldn’t be good. There were people who were sicker than I, throwing up all around me. The nurses grabbed my wheelchair and as they wheeled me back I heard a nurse say, “Sweetie you don’t have enough blood in your body, we need to start you on a transfusion right away.” I immediately burst into tears, looking back for my mom and my husband for reassurance. I was terrified of transfusions. I had only ever heard horrible things about them. About allergic reactions, and new diseases transmitted through them. I was absolutely terrified. Through my tears, (which I felt stupid for, because I figured I was old enough not to cry), the nurse quickly and quietly reassured me it would be ok. She said they’d start it slow and keep an eye on me for any reactions, and no, I wouldn’t contract any new diseases. She assured me that transfusions were entirely safe. The flurry of activity around me was overwhelming, and during a small break in the chaos I asked my husband to take a picture of me because I wanted to see what I looked like.
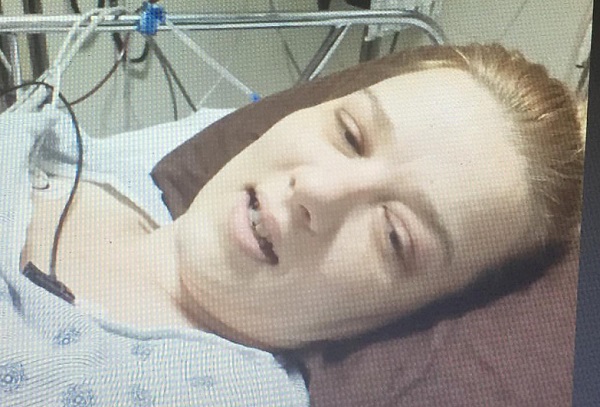
My husband hates that picture now. I think it scares him quite a bit. But I keep it in my computer files to remind me how close I came to dying that day. My skin was so pale it was almost non-existent, yet somehow I was extremely yellow. The lack of blood in my system was shutting down my organs, and I spent the next three days in the cardiac intensive monitoring ward. During this time I received three transfusions.
Bleeding to Death Monthly with No Answers from the Doctors
When I was released from the hospital, I was sent home with more iron pills and an explanation that my stored iron (ferritin) was completely non-existent. When you bleed and don’t have the raw materials to make more blood, your blood levels drop and it can get dangerous. I had no idea that I had let it get to a point where I was so close to having a heart attack from the lack of blood in my body. My doctors apparently didn’t understand it either, as they kept sending me home with little regard for the severity of my condition.
I was determined to not let it happen again. Visits to the doctor didn’t produce any new treatment plans. Unfortunately, my doctor didn’t seem to get the severity of the situation and left me to self-manage my iron and blood levels. The next month when my cycle started, I found myself back at the ER receiving more blood since I had bled out all of the previous month’s transfusions. And so started a vicious cycle: one of receiving transfusions, and starting to be okay and gaining some life back in me, and then starting my cycle, and losing more than the transfusions had given me. For the next 5 months, it became a bi-monthly habit to visit the ER, get my blood replenished and be sent home.
Uterine Artery Embolization to Stop the Bleeding: Pain and Other Problems
Finally, in March of 2014, a new ObGyn suggested a Uterine Artery Embolization again. It is a procedure where they go in through your femoral artery and place plastic pellets to shut off arteries to fibroids and other areas of your uterus. By this time the scans showed I had “innumerable fibroids”. Knowing that the UAE would probably remove the possibility of me ever being able to have a child naturally, my husband and I discussed the pros and cons and made the decision that I needed to have this done. Bleeding to death every month just wasn’t worth it anymore. So, a couple of weeks later I underwent the most painful surgical experience of my life. Imagine giving your uterus a heart attack, by cutting off its blood flow. The next 8 hours were a blur of holding my belly and crying and looking for my mom to help me breathe through the intense contractions that didn’t let up. The pain medicine didn’t even touch a fraction of the pain. Finally, at 12 hours the pain let up as my body learned how to reroute some blood flow to keep my uterus alive, while keeping the blood vessels to the fibroid tumors shut off. I went home to recover, believing it was done. I was looking forward to more normal cycles and healing my missing nutrients and blood I had lost during this whole ordeal.
Unfortunately, that was not to be. Five weeks after the procedure, I began to hurt severely and ended up passing a fibroid that was 3 inches long. This sent me once again to the emergency room where the bleeding became enough to require another transfusion. I was devastated and I just started sobbing. I knew at that moment it hadn’t worked. The next 10 months were a blur of doctor appointments, firing awful doctors, and finding new ones that were going to fight for me. That started the bi-monthly appointments of iron infusions, as they figured out what to do with me. By the end of this, my veins were so messed up that it was hard to get a line in me, and the infusion/chemo nurses were talking about putting in a PICC line. I remember looking at my husband after an infusion that took three attempts to get an IV line into my body, and saying, “This isn’t worth it. I can’t keep going like this.” At that point, we realized that we would have to give in to the hysterectomy that doctors were now recommending.
Hysterectomy and Oophorectomy: From the Frying Pan to the Fire
On January 15, 2015 I went in for a laparoscopic assisted vaginal hysterectomy, believing I would come out with one, or both ovaries. I had left the decision of ovary removal up to my surgeon, who assured me that he would leave them if they were ok. The first question I asked as I woke up was, “Do I have anything left?” The nurses refused to tell me, and once my husband was allowed to see me he shared with tears in his eyes, “They had to take everything.” Evidently the doctor had found endo and new hemorrhagic cysts on both ovaries and had decided it wasn’t worth keeping them. I was a bit concerned when I received this news, but figured menopause would just make me a bit hot and cranky. Everyone goes through menopause, so why couldn’t I? I figured I’d slap a hormone patch on my behind and be good to go. I remember looking at my husband and saying, “It’s over. We did it!!” I now feel so incredibly stupid looking back at that statement. Little did I know, I had just jumped from the frying pan into the fire.
Oh, how I wish I had stood up for my ovaries more that day. What I didn’t know then, but know now is that the ovaries control EVERY SINGLE function in my body. And being a medication sensitive person, so far none of the hormone replacement therapies are matching or helping my body. I seem to absorb and process them differently. Post hysterectomy, we discovered I had a gene disorder called MTHFR, where my body doesn’t handle and process B vitamins correctly, which leaves my liver and system overworked without the correct supplements to help it. We also learned a year later that I should’ve been diagnosed with Polycystic Ovarian Syndrome (PCOS), but that had somehow been missed between the endo, fibroids, and bleeding to death. Had I received correct hormonal labs and evaluation and had the PCOS been caught. I might have been able to receive some specialized treatment that maybe would’ve helped. Maybe…
Two and a Half Years Post Hysterectomy
I am two and half years out from my hysterectomy. I am still working on finding a stable and suitable hormone replacement (which some days feels impossible), but I’m hanging onto a sliver of hope it can be done. There are very few guidelines for hormone replacement after a hysterectomy for MTHFR or PCOS, so I am finding the challenge more often than not, completely overwhelming. Most days, I have symptoms that I never had before, which are keeping me bedridden. Migraines, body aches, and dizziness that keep me sidelined are the horrible consequence of taking out my ovaries and losing my hormones. As I began researching, I realized that ovary removal can be absolutely devastating to women. There are over 400 bodily functions that need those hormones to work properly, and my body wasn’t tolerating any of the pharmaceuticals that are available. There are days I wish I had never woken up from that surgery, and the isolation and loneliness of the situation I’m now in, leaves me in tears most of the time. My marriage of 17 years is still surviving, but it has taken a big hit. Intimacy is not what it once was, and the stress of caring for a chronically ill spouse can take its toll on anyone.
I Am Not Alone: The Sad Reality of Women’s Healthcare
The more I researched, the more I realized I wasn’t going through “natural” menopause. I was in something called surgical menopause, which in reality is just another word for female castration. I went searching for information and support sites for surgical menopause, but I kept coming up empty-handed. There just isn’t that much information or support available. So out of desperation and getting tired of calling the suicide hotline, I started a group on Facebook called Surgical Menopause Support. I brought about 15 people from my pre-hysterectomy group with me, so that we could talk about the struggles and hormone craziness we were dealing with, without scaring other women who were facing hysterectomies themselves. I figured I was an exception rather than the rule. The group has now grown to over 1,100 members from all over the world, and I’ve had to add two administrators to help me oversee the group.
Women are desperate to find out what has happened to their body, and why they are feeling so sick and miserable. I was shocked; I wasn’t the exception, this is what it is. This is what happens when you remove an entire organ system from the body. There are days when my jaw just hangs open at the stories these other ladies share, or the comments they get from their doctors. It makes me so sad. Some days I am so angry at the medical community for doing this to me and other women, without the ability to put us back together. It’s probably one of the hardest things you can put a woman through. It seems to remove so much of the person she once knew. And women are in no way made aware or prepared for the challenges that could come from this surgery. It just blows my mind.
So for now, I continue to strive to find hormones that let me be the best me I can be; hoping that I will end up being more functional than I am now. I will continue to offer a supportive place for women to chat about their struggles and feelings. My goal is to somehow make the doctors and medical community more aware of what they are actually doing to women. I hope that scientific research and funding can be put in place so that researchers can figure out how to keep women from needing this surgery at all, or at least how to replace all the hormones their bodies lose. The pharmaceuticals we have now are not enough. Some women can’t handle the bioidentical hormones and need synthetic. Some women can’t handle the synthetic and need bioidentical. There are not enough options for customization for women to pick from. The medical community must think it is one size fits all for all ladies. Something needs to be done, because other women who have had these surgeries as a necessity like I did, will find themselves in a surgically induced, new medical situation, with not much support or help. It has to stop.
This article is in honor of Mary Brite, who over the years constantly encouraged me to write and share my story.
We Need Your Help
Hormones Matter needs funding now. Our research funding was cut recently and because of our commitment to independent health research and journalism unbiased by commercial interests we allow minimal advertising on the site. That means all funding must come from you, our readers. Don’t let Hormones Matter die.
















There’s a procedure called Acessa to treat fibroids that doctors don’t tell you about because a hysterectomy is more money and this procedure isn’t covered by insurance. Everyone that has fibroids should look this up it’s minimal invasive practically no huge scar the fibroids just shrink and your body absorbs them away. It’s a miracle.
Thank you for the information. It seems like an interesting procedure that might work for one to two fibroids. However not being covered by insurance makes it out of the reach of most people. And in my specific case with innumerable fibroids, it most likely wouldn’t have been an allowed treatment. Very interesting and great to know. Thank you.
I’m at the beginning of your journey. I was diagnosed with endo in 2006. My folic acid is not absorbing. I’m recovering from my second iron transfusion this weekend. My body it really tryjng to reject it. The lvn had so many troubles getting the needing in for the transfusiin. Thanks for sharing your journey. I’m hurting all over and lost what to do next. My obgyn put me back on birth control to stop the bleeding. I’m scheduled for surgery on 9/15 to check for any polyps. So much is unknown currently how to treat people like us!
I’m sorry to hear you’re not struggling too. Folic acid is synthetic. You need folate and there’s supplements out there with folate instead ornate folic acid. Hang in there. I hope they figure out what to do to stop your bleeding. Sometimes it leads to getting the uterus removed but if you can hang onto those ovaries. They manage all your hormones.
Sorry about the typos. My fingers are numb today. Lol
Stacey you need the following tests serum & vitamin b12 ,MMA & homocysteine,vitamin D ,magnesium rbc.Your numb fingers are nerve damage occurring not carpel tunnel like most diagnosis.If your serum b12 is below 500 you need vitb 12 & folate supplements now.View videos on b12awareness.org for life changing facts.
Thank you Marilyn. I have had all those tested. And I’m now on Homocysteine Supreme supplements. My homocysteine is normal now and b12 looks good. But a couple of the other B vitamins and now vitamin E is off. So I am working on those. I still get tingling. It seems to happen a lot when my hormones are fluctuating up or down with the hrt. My best guess is that it is the veins expanding or contracting. And I’m sure I need Progesterone to protect the myelin sheaths of my nerves. But since they can’t find an estradiol hrt that I can tolerate it’s been hard to add in the Progesterone. It’s a maze. ?
I’m so sorry you’re dealing with this. If your folate is low you should take folate not folic acid. Folic acid is the synthetic version of folate. The iron infusions can be rough. I got one called Feraheme? I think. It’s been awhile. But that one seemed pretty easy compared to the others. It was an injection vs hours of sitting there waiting for a drip. Hugs and love for your health journey. ?
Thank you for being so brave and stepping up to share your story Stacy ,
Why doesn’t anyone blame “the pill”? It seems that could be the thing that started this health decline in the first place. So many women start taking the pill at such a young age when we were pretty healthy. The pill itself is a major hormonal drug that interferes with our natural healthy hormones. Then there’s the feminine products that leech toxins directly into our sensitive areas. Ten or twenty years later and we are literally dying. Don’t mess with your hormones. But it’s too late. We have to inform the next generation before they end up where we are. The Pill is evil. Read the package insert.
I understand your point in placing blame on the pill. For me the best years I had were on a low dose pill. I feel they regulated things drs could not. I do know now that estrogen sort of “robs” you of you b vitamins and now that I’m on hrt I need to make sure I stay on top of that. For me the problems started when I got off. My body could never regulate on its own. Unfortunately some of it is genetic. My mother had the same issues and an early hysterectomy. Fortunately for her it was done quickly and she responded well to hrt. I don’t feel there’s any one place to point blame here. genetics, environment, genetic processing issues, PCOS, trauma it all snowballed into a mess that wasn’t controllable with today’s research or medical treatment. Unfortunately ?
Stacy, I’m sorry for all you’ve been through! It’s a shame you got such poor medical care. That seems to be the norm in Gynecology. I also had a hysterectomy and oophorectomy / castration, both of which were totally unwarranted. All my gyn should have removed was a benign ovarian cyst. It’s disgusting how gynecologists are so cavalier about removing our organs and then dismiss the horrific after effects and abandon us. There are numerous studies dating back as far as the early 1900’s that show the incredible harm. Yet they keep doing it and no one seems to care. I’ve written a number of articles on this subject here on HormonesMatter – http://www.hormonesmatter.com/author/ws/. Feel free to reach out to me via email if you’d like.
I’m so sorry to hear you’ve had issues too. I will
Definitely go read your articles. I’m am
Glad however to have another female using her voice to help improve things. So awesome. ?❤️
Thank you for the support. Yes Women’s Health has a great need for more evolving. I hope bringing awareness to it will help ❤️
What a beautiful testimony to your strength and perseverance through an unimaginably painful journey. I’m proud to know you!
Thank you Jamie!! ❤️❤️
Thank you for sharing your story, Stacy. I’m sure it will empower more women in their health journey.
Thank you Barbara. I really hope so.
So what are the causes of heavy bleeding? I always understood it to be hormonal and there would be other ways to treat other than surgery or hormones which I couldn’t tolerate and ended up with uterine oblation because dr said it wasn’t hormonal.
There are a lot of reasons for heavy bleeding. I would say 99.99 percent has something to do with hormones. Because even if it’s a fibroid or endo, it’s usually grown because of hormonal
Imbalance. Obviously some people can have bleeding with non hormonal
Issues like blood clotting disorders or cancers. Why Drs need to do and have better tests for diagnosis.
I have endo, a bleeding disorder and a blood disease. I have vitamin deficiency and an auto immune disease. Was diagnosed with RA at a very young age.
I had PE 5 yrs ago and almost died. Diagnosed 2 yrs ago with sleep apnea.
Sometimes I’m tired of fighting, but I know I have to for my kids/granddaughter I’m raising.
Thanks for sharing your story. ❤
As it states in the article it may be nutrient deficiency – along with low levels of progesterone which is necessary to maintain the uterine lining and to prevent miscarriages. We have been exposed to so many xenoestrogens in our environment that the ratio between estrogen and progesterone is way off. Hormone tests generally show levels and not ratios – and that is why so many women have “normal” results… yet they still feel bad.
You’re correct. It has also though made my estrogen off. Pre hysterectomy estrogen labs only show my estradiol at 30 which is prettt low for someone early to mid 30s.
As Stacy mentioned, there are many causes. A few overlooked causes are anemia and hyperglycemia. Anemia can actually cause heavy bleeding (and be caused by), it goes both ways. Basically, in an anemic state platelets don’t work as well. Also, the blood vessels to the uterine lining get poor signaling which further enhances the bleeding. Here is a study that explains the mechanisms at play. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3320130/
Hyperglycemia is another overlooked cause. Hyperglycemia (high blood sugar) interferes with hypoxia inducible factor (HIF). The more of this you have, the faster you heal and cut off the bleeding.