I want to talk about a pain syndrome that most women have probably never heard of, but affects nearly 14 million women worldwide. It affects all races and ethnicities with Hispanic women suffering 80% more than other groups. It is a pain syndrome that those affected are reluctant to share with their partners, closest friends, or their doctors. This is because their pain revolves around and within the vaginal area, an area that we women often do not feel comfortable talking about in any company. Making this the “silent pain syndrome” and leaving women everywhere feeling alone and damaged.
This pain syndrome is known by a few names such as Vulvodynia, Vestibulitis, Dysaesthetic vulvar, vestibular adentis and vestibulodynia. It was given several names back in the 1980’s to help doctors refine and come up with treatment plans based on where the pain was located, the condition of the tissues in the vagina, or surrounding areas, as well as what provoked the pain. However, since the 80’s more and more studies have been done on the condition showing that most women who suffer with it have overlapping symptoms from one form to another. This has lead the medical community to start moving away from trying to categorize or compartmentalize it into one of these diagnoses. For the most part nowadays, it is just called vulvodynia.
Vulvodynia was recognized as far back as the 1800’s, when it was treated by surgically removing the vulvar area. Unfortunately, many of these women only got temporary relief. It unfortunately, was left out of the medical books until the 1980’s when Dr. Edward Friedrich began reporting on it. Since then 80 studies have been done on the condition. It is not clear whether the increase in research is due increased awareness or an increase in the condition itself. The National Vulvodynia Foundation says that the average women suffering with this condition can see upwards of 15 doctors and it can take as long as 12 years to receive a correct diagnosis. This is because so many doctors are still ill informed and poorly educated on vulvodynia. The medical community is lagging in research when it comes to women’s health conditions, especially those that cause chronic pain in our genital areas.
Sadly, most doctors will push their patient’s pain syndrome off as a psychological problem, PMS, stress, lack of love for her partner or even sex in general. Many of these women find no help from the medical community and go on to suffer in pain silently, leading to other co-morbidities such as depression, anxiety, suicidal ideation, irritable bowel syndrome, interstitial cystitis and fibromyalgia. For many women who have been abandoned by the medical community, they will go on to question their own mental and emotional stability. They will often blame themselves for their condition, thinking they have somehow damaged their body physically through picking up an unknown STD or have psychologically thought themselves into this pain syndrome as many of their doctors have suggested. These women often are unable to continue having sexual intimacy, some get so bad that they reach a point of not being able to wear clothes, sit, walk or even tolerate a gynecological exam. Urinating or defecating can bring on horrific stinging pain that leaves many to cry out with the simple act of going to the bathroom, which in turn leaves them drinking less and eating less and holding their urine or bowels for as long as they can so as to not experience that feeling. Unfortunately, doing some of these things can further the progression and pain from this syndrome as well as to create other dysfunctional conditions. For those women whose conditions continue to progress, they can be left extremely disabled, unable to work or care for their families, which in turn leads to high divorce rates and financial losses. Couple all of that with a condition that a woman feels she has no one to share it with and it is no wonder that they often go on to suffer with depression, anxiety and suicidal ideation.
What is Vulvodynia?
Vulvodynia is known as a neuropathic or inflammatory pain condition to the genital area in women. As of yet it is caused by an unknown etiology. It is thought to be from the same family and act much like “phantom limb syndrome”. Vulvodynia causes a myriad of symptoms such as inflammation, redness around the vestibule (opening to the vagina), the vulva itself (outside vaginal lips also known as the labia major) and to the inner or small lips (also known as labia minor), as well as the vagina itself (the inside tissues). It can effect specific spots in or around the vagina, like the perineum, rectum, thighs, pubic bone or pubic hair, clitoris and the urethra. For some women it can affect all of these areas making their situation life altering, disabling and agonizing. Women who have this condition experience stinging, burning, itching and razor cutting like sensations with the slightest of touch, making intercourse, tampon insertion, wiping or washing the area and the wearing of clothes painful to impossible.
Some women also complain of feeling as if they are dried up down there, while others feel as if their insides are falling out of them. Often when the clitoris is involved, it can cause agonizing pain that shoots up into the abdomen. In many of these cases, the women’s abdomen can become inflamed and reddened as well, leading to irritable bowel syndrome symptoms. For many the pain is so agonizing that they are left unable to wear clothes, walk or even sit. For some the pain can extend into the urethra or even the bladder setting off another pain syndrome known as interstitial cystitis. This condition can leave them in severe burning pain during and after urination.
Vulvodynia is unique to each woman with some having it constantly while others have it intermittently. Some will only suffer from specific areas of pain while others have it everywhere. Some will only have pain with intercourse while others have it with anything entering or touching the vagina. Some will suffer with only hypersensation while others will suffer with all of them. For some the pain will be manageable while others it will be life altering. Each women’s pain level and frequency is different making this illness hard to understand and even harder to treat.
What Causes Vulvodynia?
Well that is a good question, and unfortunately, no one in the medical community has yet been able to answer. However, there are several theories about what increases the risk for developing vulvodynia.
Compressed Pudendal Nerve
We know that some women have a damaged, compressed or pinched off pudendal nerve. The pudendal nerve is a nerve that comes off the spine and innervates the pelvic floor region. It is what allows you to control urine flow or bowel movements. It is also, what activates your glands when aroused to produce the moisture in the vagina and allows you to have an orgasm. It has many important and enjoyable functions, but if it becomes damaged it can also create a lot of pain, dysfunction, and grief. Damage to this nerve can happen by a fall to the back or butt. It can be injured during labor. It can become inflamed or compressed by an arthritic condition or by a cyst or tumor. Some of these conditions can be fixed with surgery or nerve blocks, which in some instances may relieve the vulvodynia. Unfortunately, compressed nerve affects only a small number of vulvodynia sufferers.
Infections
It has also been shown in studies that 54% of all women with vulvodynia also test positive for HPV, however scientists has not been able to say with certainty that this specific viral infection is the cause for these women. Instead of it being the cause, it may just be the women’s own immune response to the infection. Researchers have also studied other viral infections that are known to cause neuralgic pain syndromes like this, such as cytomeglavirus and the herpes viral family, but have not found any evidence of these infections.
Researchers have looked at candidiasis infections as well; this is because so many women with vulvodynia have a long history with chronic fungal infections with many using repeated “azole” therapy to treat it. Yet again, they have not been able to find a link or correlation with any species of fungi. Although there is a question as to whether the use of any of the “azole” drugs could have possibly caused this condition or whether it is just associated with it because so many patients with vulvodynia are misdiagnosed with yeast infections. Due to this, the medical community warns women to be careful when using the OTC “azole” drugs and to follow the manufacturer’s recommendations. Additionally, if the yeast infection is not cleared with the usual course of treatment or a second infection develops, you should not use the cream again without first seeing your doctor.
Studies have also looked at bacterial infections as the cause, here they found that 17% of sufferers had an infection with what is known as ureaplasma, which is often seen infecting the Bartholin glands. For these women treating the infection often times cleared the vulvodyina. They also found a small number of women with the Streptococcus B infection and again in many of these cases, treating the infection cleared the vulvodynia. None of these studies have been able to state with certainty that any particular infection is the cause, but they do show that if you suffer with a long standing, chronic or hard to treat infection of any kind (viral, fungal or bacterial) you could be at a higher risk of developing vulvodynia.
Childbirth and Episiotomy
For other women there was no clear accounting of an infection but they could relate the start of it back to the birth of a child or the episiotomy. Here again we are looking at damage to the nerve or the soft tissues.
Hormonal Birth Control, Cancer Medications and Other Steroids
Other studies have implicated oral contraceptives and early childhood intercourse as a cause, both of these may be linked to hormonal imbalances. Some drugs have been implicated as the cause of it too, such as cancer drugs and both oral and topical steroids. Even though the topical steroids are used to help with the inflammation and itching in this condition, they are known to cause thinning of the tissues and sloughing. They tend to lower the immune system allowing for other infections to pop up making the situation worse.
Comorbid Fibromyalgia and Chronic Pain
Fibromyalgia has also been implicated in vulvodynia, mainly because so many women who suffer with fibromyalgia also suffer with vulvodynia. However, it is believed that fibromyalgia is due to an unknown muscular etiology and as if often seen alongside chronic fatigue. Both of which are thought to be caused by an abnormally high level of a neurotransmitter involved in pain sensation, so having this pain syndrome alongside of these would stand to make sense and put you at a higher risk for vulvodynia.
Oxalates
Older studies have suggested high oxalates in urine may be responsible for the pain. Oxalates are like little sharp slivers of glass made up of calcium that are excreted through our urine, but as of recently this theory is no longer being considered. This is because so many women have not tested positive for excessive oxalate output. Those who have gone on low oxalate diets have had some to no response, leading the scientific community to suggest that the oxalates themselves are not the problem but instead the fragile irritated tissues that the oxalates cross are more the issue. Now even though this may not be the cause, going on a low oxalate diet may be worth a try to lessen the pain. Another study suggests pH imbalances may be involved, but again cannot be confirmed as of yet and does not hold true for every women.
Inflammatory and Allergic Reactions
Recent studies have shown a correlation with inflammatory allergic reactions, like those seen in people with mast cell reactions. This is also seen and been implicated in interstitial cystitis too. However, we are still in the beginning phases of understanding not only this correlation but also Mast Cell Disease. If you suffer from this, you may be at a higher risk of developing vulvodynia as well.
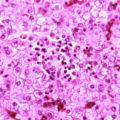
Researchers at John Hopkins in Baltimore looked for two cytokines (immune stimulating cells) associated with inflammation. They found significantly higher levels of interleukin 1 beta and alpha necrosis tumor factors in test subjects. This would suggest that there is an inflammatory process going on, possibly due to an autoimmune problem. Then pathologists out of Rotterdam in the Netherlands found through biopsies chronic inflammatory infiltrates in all the patients and none in the control group. The infiltrate was composed of T-Lymphocytes as well as a small number of B cells, plasma cells, mast cells and monocytes. An immunoglobulin important in antibody reactions, IgG was found in plasma cells of 75% of the patients. This again suggests that there is an inflammatory process caused by an autoimmune reaction going on, however, they are not ready to confirm or deny this yet.
Finally, the University of Iowa has found impaired natural killer lymphocyte activity in the women effected as compared to a control group. Natural killer cells are needed to defend the body against certain cancers, so this finding may explain why some women with vulvodynia also suffer with dysplasia, despite having not contracted the aggressive cancer producing HPV strains. This finding may bring us back to implicating the HPV virus. However, this is all new information and nothing has been confirmed yet.
Diagnosing Vulvodynia
There is no specific test for this condition. It is diagnosed by ruling out other conditions and diseases. Physicians may want to test and treat for any infections first and see if that relieves the pain. If not, then it may be vulvodynia. Vulvodynia is frequently misdiagnosed as a chronic vaginal infection from fungi or bacteria. However, if your cultures are negative for an infection you may want to consider vulvodynia.
Treating Vulvodynia
This is the million-dollar question that both women and vulvar pain specialists are asking. Unfortunately, we really do not know what causes it. This means that without an identifiable factor, we are guessing at how to treat it. We also know that every woman experiences vulvodynia differently, making a “one size pill” that treats everyone impossible. Each woman will go through a trial and error with treatment modalities. This can often make the journey long and tedious, as well as, quite discouraging and even painful, especially when something heightens the pain instead of lowering it. This is why it is very important to get involved with a vulvar pain specialist, not just a pain clinic or pain doctor, but one that has been truly trained in treating this condition. Here are some of the many modalities in the arsenal to treat vulvodynia.
- Trigger point injections. This will numb the area for a few hours to days, giving some relief with the hopes that they will be able to shut off the nerve or reprogram it. Lidocaine is usually used for this. However, this procedure can be quite painful and risks damaging the nerves and tissues further, so for many women this is not an option. Now some doctors will also prescribe lidocaine jelly or even xylocaine jelly to be smeared on the painful areas. These can topically numb the tissues and nerves, giving some minor relief for a few hours. Although once again, for some women just putting this gel on can be too painful and does not last long enough to make it worth it.
- Topical steroids. These are often prescribed to help with the itching and inflammation, even though research has repeatedly shown them to be ineffective.
- Baking soda douches. If the vagina is too acidic, some doctors will recommend baking soda douches, which is non-toxic and in a few cases, it can help.
- Interferon. Several studies have tried treating women with interferon. This has shown some success, but the relapse rate is very high and one study showed that using interferon on women who do NOT have HPV actually worked better.
- Topical estrogen creams, progesterone and/or testosterone. Early research was promising. However, it may be painful for those women who cannot tolerate any kind of a cream placed around or in the vagina. It is important to note that estrogen cream can activate Mast Cell Syndrome.
- Prophyllin compresses. Some women find compresses made of prophyllin ( a prescription powder) to be soothing to the area.
- Low oxalate diet. Oxalates are in nearly everything we eat, but you can avoid the high oxilate foods. Doctors who prescribe this diet often times prescribe calcium citrate to go along with it. The calcium citrate helps to neutralize the oxalates in the urine. The Vulvar Pain Foundation reports the two most consistently helpful regimes for their members are the estrogen creams and low oxalate diet with calcium citrate. Another thing that sufferers report helping them is, drinking lots of water. Water dilutes the oxalates in the urine which decreases irritation.
- Anti-depressants and anti-convulsants. Fibromyalgia researchers have suggested that certain anti-depressant drugs may be useful in women also suffering with FMS. Vulvar pain researchers have not done studies, however, clinical experience; they suggest that the SSRI’s are not effective in treating this condition. There is no research on the anticonvulsants.
- Capsaicin (an extract of the red pepper). Capsaicin has been used successfully in other neuralgic pain conditions like, diabetes, HIV, herpes infection and even in interstitial cystitis. An ongoing study of topical application suggests it may relieve pain, however, because Capsaicin produces significant burning when applied it may not be appropriate for those suffering with vulvodynia due to inflammation. It may not even be appropriate for those women with skin break down or seriously sensitized tissues.
- Opiates and other pain relievers. These may be effective in the short term, but long term they are problematic.
- Physical therapy. Specialized pelvic floor therapy has helped some women suffering with vulvodynia, especially those who also have FMS. Dr. Glazier, a psychologist from New York, states that biofeedback along with physical therapy to the pelvic floor can help to strengthen and relax the muscles in women with vulvodynia. This therapy is often also used in people with interstitial cystitis and irritable bowel syndrome too.
- Surgery. There are multiple surgical options but none appear to reduce the pain and many increase it.
- Cannabis oil. Cannabis oil applied topically has become all the rage, but as of yet, there are no studies to evaluate its effectiveness. Vulvodynia sufferers, however, report significant relief .
What is the Prognosis with Vuvlodynia?
I wish I had better news to report here and maybe one day I will have it, but for now this is not known as a curable condition. Do not be discouraged. We have many diseases that we are not able to cure but have the ability to effectively control. The first step is getting properly diagnosed and ruling out any other conditions or infections. The second step is finding a vulvar pain specialist or a vuvlar pain clinic to start the treatment process. Both of which can be found through your doctor or through the National Vulvar Pain Foundation. Once you reach this point, your journey to getting better will begin.
Please know that it may take quite a while to reach a point of lessened or no pain. It may also take several attempts at different or mixed modalities including medications, creams, diet, physical therapy and trigger point injections to find what works best for your condition. If you are also suffering with depression, anxiety or suicidal thoughts then you also need to find a psychologist to help you work through all of this as well. Please know that these mental and emotional conditions are very common in women with vulvodynia. This is due to many factors such as constant pain, loss of intimacy and all that goes along in a relationship because of it, including, a loss of self-sexual beauty and feeling damaged. Suffering in silence also causes distress. So, please if you take nothing else away from this article, just know you are NOT ALONE!
We need your help.
Hormones Matter needs funding now. Our research funding was cut recently and because of our commitment to independent health research and journalism, unbiased by commercial interests, we allow minimal advertising on the site. That means all funding must come from you, our readers. Don’t let Hormones Matter die.













I experienced vuvladynia for 2 years. It is a long story but I eventually got diagnosed after 2 years. I tried loads of things that never worked and eventually I found that stopping my contraceptive pill worked. Mine was clearly triggered by my hormones. I don’t know if this will help anyone else but I hope it does.
How long did it take for it to get better after getting off the pill? Did you have a hormone issue?
I have been suffering for over a year with vulvadynia. I am 70 years old and terrified of hospitals and doctors. I haven’t been for a diagnosis but tried everything available over the counter. I have good days and very bad days I don’t know where to turn next I can’t go and be prodded and poked over and over Please anyone help
Hello,
My gynecologist put me on Gabapentin 300mg 3 times a day for my persistent vulvar pain. I was put on this medication only after all of my tests came back negative. It has helped a great deal with the pain and burning. I have an appointment with a vulvar specialist in about a month. I have only been able to speak with scheduling personnel. Perpahs you can answer my question? Is the vulvar specialist going to be able to do a complete exam even though I have been taking Gabapentin? Also what is usually done for this kind of exam and what kind of tests are usually done/ordered? Thank you for any help!
Mine is caused by a tight pelvic floor. My pelvic floor is tight because of a misplaced coccyx due to injury. When i get pelvic floor massages and treatment it helps quite a bit. I’m waiting to get the tailbone adjustment soon. I’ve suffered for 16 years and am just now learning that many of my issues stemmed from this.
Ladies, please know that it flares up and gets better. For me, I also have a slight bladder prolapse because of the spinal issue. Everything works but is pushed in the wrong place. I do have pain wearing pants but there are good and bad days.
Sometimes a pelvic adjustment with a chiropractor helps. My advice is to seek pelvic floor treatment, chiropractic help for pelvic misalignment and tailbone exams. Most women (especially though who have had a vaginal birth) have a prolapse of a pelvic floor organ. We are not ‘hysterical’. We do not need antidepressants or nerve blocks. We need the nerves be less stimulated, not impinged and to heal. Good luck to you all.
I’ve had vulvodynia for 6 months. In reading the treatments listed above, if one could call them that, one finds they can expect: extremely short term relief, ineffective, helpful “in a few cases,” high relapse rate, may be painful or activate Mast Cell Syndrome, soothing but could only be used in private, the oxalate thing has been pretty widely debunked though that’s not mentioned here, not studied/not effective, extremely painful, only effective in the short term, finally a helpful one!, does not appear to reduce pain and might make it worse, and another untested suggestion. Then I see in a response that the longer the pain continues, the harder it is to break since your brain has become rewired and the pain can also spread. So this is a life ender, isn’t it? The best I can hope for is mere existence. WHY ARE DOCTORS STILL PRESCRIBING THESE TREATMENTS?! I was prescribed an antidepressant and when I asked why my doctor felt they’d be helpful since all the papers I’ve seen says they’re no more effective than a placebo, she had no answer. She said it “could help.” What I’m reading here is that no one can help me, but they’ll keep stringing me along, charging me a fortune for things they already know are not effective. I’d like to know the suicide rate among sufferers. We are left to try to figure this out by ourselves. Have you seen the large following for the “Medical Medium?” It’s telling that women are desperate enough to believe eating 1/2 papaya and juicing gallons of celery will cure them because a “medium” with no medical background heard about it from the spirit world.
Hi Angie I am so sorry that you have been diagnosed with this. It is an awful and life sucking syndrome that effects every area of a woman’s life including how she sees herself. I feel like I can hear your despair, pain, frustration and hopelessness in what you wrote here. I know everyone one of those feelings all too well, but I also know that women do get better and do go on to have normal intimate relationships and live “normal” lives. I am not sure where you are reading a lot of the things you are stating here, nor am I sure if you are interpreting what you are reading correctly, but I can tell you as a former patient and as an advocate for this illness and one who works with women who have been effected by it, that women do find relief from many of these treatments. Now let me say that ” no one size treatment fits all” nor do any one of these treatments work 100% especially when used alone and not with other treatment modalities.
So, when I say “no one size treatment fits all” this is the most important part of finding the right treatment for you and one that is usually only addressed by vulvar pain specialists who truly understand this disease. I can guarantee you that your Gyne has a very limited education and knowledge, if any, on how to diagnose you correctly and find the right treatment plan to help you. This is why I tell women it is extremely important for you to be referred to a vulvar pain specialist. These specialists are specifically educated in finding what possibly set off your vulvodynia, they are trained in knowing what kind of vulvodynia you have and then based on that knowledge they are educated in all the treatment modalities that would best treat your vulvodynia. These are things that Gyne’s have no knowledge of which is why your Gyne could not tell you why an antidepressant would possibly work on you. If your Gyne did not figure out why you developed vulvodynia then they also would just be throwing meds or treatments at you with the hope of something sticking, instead of knowing exactly what would work best for you. It is a true shame that any Gyne out there who has some limited knowledge of vulvodynia would not explain to you that they are not the one to help you and then refer you on to a specialist.
So, let me explain too that none of the treatments relieve pain 100% and there are several reasons for this. First researchers and doctors still to this day really do not know or understand the full reason why some women develop this condition while other women who go through the same thing do not develop it. Although they are focusing on the persons immune system as well as the make up of the persons nervous system. Hopefully in the near future they will have a better understanding which will then lead to a “one size fits all” treatment plan for women. Secondly, as I kind of just eluded to in that last statement there is more than one thing that is at play in causing this condition. Meaning that there are biologic and structural issues with a persons body. So, there may be a possible deficiency in the persons immune system or there may be a problem with the immune system being able to shut itself off after an infection has occurred and then resolved. There is also the possibility that the persons nervous system is wired differently the others. There could also be a break down within the nervous system from a trauma to the lower back and spine or even to the brain itself, so nervous system messages are being skewed up the chain from the vagina or pelvic region to the spinal cord and then up to the brains pain center. If there is a “glitch” anywhere in this chain it can set of a pain syndrome like vulvodynia. Unfortunately, we do not have the capabilities as of yet to find that “glitch” somewhere in that chain, we just do not have the imaging or testing yet, so doctors are left to find treatments that work on the entire chain, which are not as effective and targeted ones, but at least offer some help and hope. We also know that once a “glitch” in the nervous system happens, no matter where it happens in the chain, it creates a pain syndrome that begins to rewire the brains pattern. This rewiring then begins to change the entire way the brain perceives stimuli of any kind not only in that specific area, but in time throughout the body. However, there have been multiple double blind studies over the last decade and a half that have shown that with the right treatment plans the brain can once again be rewired back to a place that no longer sees stimuli as painful. One of the most promising of these treatment plans is known as cognitive behavioral therapy, which is completely different then psychological therapy for depression, so please don’t mistake this form of treatment as meaning that you need psychological help because this pain is all in your head, because it is not and the specialists know this! However, let me also say that even with cognitive behavioral therapy being one of the best treatment plans it too usually requires other forms of treatments combined with it to make it even more successful. Things like antidepressants or anti epileptic drugs or physical therapy and even diet. When everything is combined together in the treatment plan most people begin to see improvements in their level of pain and disability disappear within with about 6 weeks and can find near total pain relief within 6 to 9 months. This type of treatment is used in all kinds of pain syndromes throughout the body, not just with vulvodynia.
Now, because you are dealing with a chronic condition, just like any other syndrome or disease that can effect the body, you will have to manage it throughout your life. Meaning once you reach a point of it no longer causing you pain or disability, you cannot just stop your treatments. So, if you are taking an antidepressant you will still need to continue to take this drug to prevent the pain nervous system from becoming hypersensitive again. If you are eating a specific diet that has helped you will still need to maintain those diet restrictions so as to not aggravate the metabolic system, which in turn can set off mast cell if that is what caused your vulvodynia or irritated the delicate nerves through bladder and vaginal area, ect.. If you are in physical therapy you will need to continue to do your exercises so as to keep the muscles, tendons and tissues strong and flexible within the pelvic region, just as you would have to do to maintain any other muscles in your body that you created by working out. So, yes there is a relapse rate but only if you stop doing what made you get better. This would be true if you suffered from diabetes and stopped your diet and insulin, or if you had MS and stopped your meds and physical therapy. Vulvodynia is no different than other chronic conditions except that is not openly talked about or heavily researched because it effects a woman’s vagina, something our society does not like to openly talk about. However, if you adopt your new lifestyle of treatments and continue them as part of your daily regime as you would for any other chronic condition your chance of a relapse is lessoned to near nothing, which is why most women who get the correct treatment from a vulvar pain specialist go on to not only get better but take their lives back and lead normal pain free or near pain free lives which also include intimacy.
So, because we know there are several things within the body that cause this condition, we also know it takes more than one treatment modality to halt it. You see, they must treat each part of the body that is at play in causing this pain syndrome and that requires more than one treatment to get you better. So, please do not misinterpret studies that say that low oxalate diets have been found to be useless or pelvic floor therapy only works in the short term cause none of that is true. There are not only numerous studies that have shown that they work but there are millions of women out there have found relief and regained their lives back from them. However, none of these treatments work 100% all by themselves, which is the part you have either misinterpreted or the study has conveniently left out. Again I want to reiterate that all of these treatments will only work in the short term if you stop them once you begin to feel pain free or normal again, so you must adopt these treatments as a new part of your daily regime just as a diabetic has to adopt a new diet and insulin into their daily regime in order to maintain their health. So, yes doctors are still prescribing these treatments to this day because they WORK when used correctly and in combination with other modalities. They also work when the patient faithfully applies them to their daily life regime. This has been proven again and again through double blind studies both here in the US and in other countries. There are also millions of women world wide that gotten better and moved on with their lives. There is absolutely no reason you should “just exist” nor should you suffer in pain, we do have treatments of all kinds that have been proven to work. Please know that a double blind study means it has been tested against a group who were given placebos and those that got the real drug or treatment showed more improvement than those who did not get the real thing. Now please note that I said “it showed improvement” not that is cured them. Again this is because none of these treatments will cure you or relieve you pain 100% all by themselves. At best they will improve you pain level as well as you level of disability, when used by themselves and know that when a treatment is studied it is studied all by itself not in conjunction with other treatment modalities. So, the best the study can say is that it “improved” the patients quality of life and lessoned their pain level. Many of the studies will state that the treatment improved their condition by some percentage level. So, maybe the diet improved the persons pain by 15%, which does not seem like a lot but it means that it has benefit and for some women even a 15% improvement in their pain level is worth the world to them. Now you take that 15% improvement and add another treatment modality that has shown to improve the persons pain level by 25% or 50% and the patient now has a 40% to 65% level of pain reduction which is huge! Finally you add in another treatment modality like cognitive behavioral therapy which improves the patients pain level by 45% and now that patient has an 85% to 100% improvement in their pain level and they are back to living their life again. This is how these treatments work in conjunction with each other getting the person back to their life. These treatment regimes have been studied and followed by many large institutions as well as the National Vulvodynia and Vulvar pain foundations who over see these treatments in order to help women regain their lives.
Let me also address something else you said here, you said that some of these things can make you worse and you are right about that. There are women who go through injections or use creams that can cause a reaction and any negative reaction can cause trauma to the already traumatized area, setting off more pain. However, that pain is usually short lived and once the treatment is stopped and the area calms down you go back down to your baseline of pain. So, yes there are some treatments that you find that may make you worse, which makes finding a vulvar pain specialist all that much more important, because many times they can avoid using a treatment that may set you off and they are usually quick to get you off of it and help you recover and then move on to something else that may work better for you. I would tell you that treatments that make you worse are rare, but do happen, but I would tell you not to be afraid of trying what a pain specialist is offering because the odds of it working are far higher than you have a reaction.
On another note, there are NO treatments that will CAUSE mast cell activation syndrome, that is impossible. Mast cell activation syndrome is a condition where your mast cells break open and release histamines from things that usually do not cause a reaction. This condition is rare and usually only seen in people who have other under lying conditions like genetic connective tissue diseases like EDS or Marfans Syndrome. Mast cell activation syndrome is a serious condition that causes all kinds of serious reactions throughout the body from foods, drugs, supplements and even emotional responses. It is genetic and system break down and one that has to be treated by an immunologist / allergist and there are tests to evaluate if you have this condition. For women who suffer from this rare condition it can and has been shown to cause vulvodynia usually due to hormonal imbalances and or lubricants or even the simple action of friction to the tissues. There are effective treatments for this condition but usually are prescribed by immunologists / allergists. So, again this is another reason to be referred to a vulvar pain specialists because they are trained in figuring out what may have set your vulvodynia off and they after speaking with you and getting your health history they may find that your vulvodynia is due to mast cell in which case they would refer you on to the immunologist / allergist for treatment. so, please know you are not at risk of developing mast cell from any treatment prescribed to you.
Finally, let me explain what your doctor apparently could not. So, the reason your doctor prescribed an antidepressant is because we know that there are a select few antidepressants that have a unique side effect of “numbing” the nerve endings and slowing the nerve signals to the brain. The most widely known and used one is Elavil or also known as amitriptyline, it comes from the family of tricyclic drugs. These drugs when used in small doses (no where near the dose used to treat mental health conditions) they are very effective at reducing nerve pain throughout the body. This drug is used in people who suffer not only from vulvodynia but also irritable bowel syndrome (IBS), Migraines, painful menstrual cycles, reflex sympathetic dystrophy (RSD a well known very painful condition that happens to people after an injury or amputation), central sensitization syndrome (CCS a very painful full body pain syndrome much like vulvodynia but all over the body), myofascial pain syndrome, and the list goes on and on. This drug has been proven over and over in the treatment of pain syndromes of all kinds and it has been shown to be extremely effective when their is a “glitch” in the nervous system chain. However, it is very important that once again it is only one part of a treatment program no matter which one of these pain syndromes you suffer from. It can reduce or relieve you pain by 40 to 65% but you almost always need to add something else to it to get to that 95 to 100% pain relief. So, like with IBS you would need to take this drug plus change your diet and even add in exercise that strengthens the stomach muscles. For migraines you would take this drug and add it to a caffeine and gluten free diet along with stress reducing techniques. For RSD you would take this drug and add in physical therapy and cognitive behavioral therapy too. For vulvodynia you would take this drug and add in pelvic floor therapy, exercise and cognitive behavioral therapy. For each of these conditions the Elavil is a major part in reducing the pain, but in order to get that sweet spot of near to no pain you would still have to incorporate other modalities. This is true for thousands of illnesses, diseases and syndromes. Please know that you life is NOT over and you are NOT alone in this. There are millions of women out there that have been where your at and have regained their lives, there are also thousands people out there living with daily pain syndromes that cause depression, anxiety and disability its just that their pain is not located in the vagina, so the can openly talk about it, but you can too if you get into a support group with other women like you. many of these groups can be found on line. I would also encourage you to get involved with the national vulvodynia and vulvar pain foundation. They have lists of pain specialists in your state and maybe even your area. They have the latest and newest studies out there and participate in studies that you may be able to get into too. Their site can help explain a lot more about this syndrome too and sometimes just learning about your illness gives you back your power and control that you feel you have lost in all this. You can become an educator to your doctors and a life line to other women even while you are in treatment yourself.
Finally, let me just say that I have been where you are at many times over in my life from several different types of health conditions, but I have learned that if I allow the pain and disability to over take me I become paralyzed and remain ill, but if I learn about my condition and find others like me to talk with I always regain my power and move forward with adapting and getting better to my condition. So, I know your pain and your fear I can hear it in the words you wrote here, but I hope what I have wrote hear eases your mind some and gives you some hope and lets you know you are not alone in this or even in the way you are feeling right now. However, I want you to know that millions of women all over the world have faced what you are facing right now and have gotten better and regained their lives with the treatments in this article, but everyone of them that have gotten better have been treated at vulvar pain clinics. One last thing here, you brought up suicide and I want to quickly address this. There have been women that have committed suicide over this condition, however these are the women who sent years suffering with what they believed was an unknown condition because none of the gynecologists they seen correctly diagnosed them with vulvodynia and for the ones that did manage to get diagnosed were unfortunately not referred on to specialists who were trained in all the modalities to treat their condition. These women suffered horribly as their vulvodynia spread to incorporate their colon (IBS), their bladder (intercystial cysititis, IC) and then spread to causing fibromyalgia, chronic fatigue, migraines, painful periods and eventually central sensitization syndrome. All of this lead to full disability and pain beyond what they could tolerate, which left them alone, depressed and anxious, which eventually lead to them feeling like there was no way out of all this pain other than to commit suicide. This is sad reality for women and more so two decades ago before women and doctors began to realize that vulvodynia was a real biological condition caused by the nervous system and possibly the immune system or some structural problem with the spine and pelvis. We now have knowledge and specialists in this field and treatments that can halt this disease and return women back to their lives. we also have social media and a way to contact other women in our same position so we are not alone. So, the suicide rate has decreased immeasurably, but again it takes a good gyne to recognize the condition and refer the patient to a specialist and a good pain specialist to work with that patient on all levels to return them to their former self. When all these things come together women no longer have to entertain the thought of suicide. so, I hope if you come to a point of feeling that depressed that you get help immediately and I hope you will never get there but instead request that your doctor refer you on to a specialist and definitely try that antidepressant because it will definitely help you, just know it can take about 6 weeks to see the beginning effects of it and know that it is only one part of what you will need to get better, but it is a good starting point.
Well I know this has been long but I hope it has helped you. I wish you the best
Let me also say a few
Thank you for this considered and kind reply. I know I sound angry. I am angry. If I may follow up with a question – how does one find a vulvar pain specialist? I’ve seen a urogynecologist, an allergist, a dermatologist, a chiropractor, a general practitioner, a physical therapist (none of the afore mentioned knew anything about vulvodynia), and most recently, “The Midwest’s leading expert in sexual medicine and vulvar pain” who is on the NVA’s list. The latter is the person who told me to take the meds and said it “hurt her feelings” that I would ask for names of doctors who could rule out other problems using MRI, etc. She does not view this condition as best handled with a multi-disciplinary approach.
You’ve been very kind in your response and I appreciate that.
Hi Angie, I am so sorry that you have had such trouble finding the help that you need. It was quite obvious that you were angry, frustrated and feeling hopeless by what you wrote and I am sorry that you are feeling this way but get why you are in the place with the trouble that you are having finding the help you need. So, usually your gyne should be able to refer you to the closest pelvic pain clinic in your area, but if your doctor does not know this information then the next step is to use the NVA’s list, which you did. So, let me ask you this, you said you went to the leading Midwest sexual and vulvar pain expert, so I am assuming here that you live in the Midwest, so can I ask what state do you live in? Let me also say that not all pelvic floor pain specialists are the same and one that is not part of a clinic may not be the best one to go to, I don’t care if they do think or are listed as the leader in the Midwest. I also have problems with doctors that discourage or get upset when a patient wants a second opinion, most good doctors relish a second opinion. So, you obviously need to find another doctor and I can try to help you find one, I just need to know what state you live and if you are willing to possibly travel? Also you said originally that this all started 6 months ago, so can I ask do you know what proceeded the onset of your pain? Like did you have an infection, or suffer an injury to the pelvic area or lower back, or did you give birth? This can be a big a clue in why you developed this and it can lead to a better treatment plan. Well, let me know where you live and I will see if I can find a better doctor or clinic for you to see.
Sincerely, Debra
Thank you, Debra, so much. I’m in Nebraska and could travel. Onset was in June, but there was no notable event leading up to it. It was an overnight change. No recent infections and no injuries. I have had one vaginal birth, 10 years ago, and it was problem-free. The only possibly unusual things I can think of are that I went off hormonal birth control in January (after 20 years on…with a 2 year gap to have my baby) and that I have mild scoliosis and a tilted sacrum. My estrogen level was elevated, testosterone was sort of low, and FSH was normal when tested. The physical therapist I saw said I have weak hips, as well, which is actually what I’d asked to vulvodynia specialist about, as I wondered if a musculoskeletal issue was the root cause. She said it hurt her feelings that I’d ask to see another doctor.
You’ve listened and taken your time to offer me guidance, and that is more than anyone else has done. It’s the greatest kindness I can imagine right now. Thank you.
hello,thank you for this article. im trying to read about all and i cant find an answer still,for sure.
the problem is with my daughter. she is only 12.suffers from vulvodynia from June this year. I cant tell more about her life: she trained swimming in high chlorinated pool in our town,we live in Serbia,ex Yugoslavia. She trained for 3 years,wearing costumes of synthetic material. 6 days a week, 1,5 hour – training. After training,she wash her long hair with shampoo (Nivea, or something like that),and using Conditioner,every day….
Some symptoms of pain we noticed 2x last year,every time in the pool.We didnt know what it is back then.
This year,because of corona,we were in carantine for 3 months,so she couldnt swimm. After she was back on swimmingpool, after 3-5 trainings she was in pain. pain: burning, stabbing, itching…. etc. We went to one gynecologist in our town on ultrasound,she told us ,all okay. I asked how okay if she in pain. She said to me, you are very protective mother, you are seeking something that doesnt exist, the kid is healthy, she will get her first period. I said okay, and we found other gyn.in other city, where she did some exams, there wasnt yeast infections, all is okay in ginec.way, but as she is suffering still – she told her its vulvodynia.
We were at neurologist, all okay, all in private clinics,
then to alergologist, no allergies, blood is very well, urine okay, all…
So,we dont know what to do anymore,she is just a child,needs to go to school,but she cant go sometimes.
Its very bad situation – and she still suffers.As a mother im concerned what will be with her health. She stands it all, but its not normal.
She cant stand no creams to put on vulva, because of burning.
We dont have some specialists here, we are in dark. She is just a little kid,and she wants to live. How can i help her?
Hi I am so sorry that your daughter is going through all this. There are few things that come to mind that you may want to check out. So, my first thought is that she may actually be suffering from one of the rare types of fungus infections, like Glabrata or Tropicalis. These are rare forms of fungal infections that can infect the vagina and are quite often seen in people who wear bathing suits for long periods of time or have taken antibiotics. so, these types of infections cannot be detected on the “normal” fungal or bacterial vaginal infection tests. Your gyne would have to order a “rare fungal identification culture” now this test requires a special swab and the swab is put into special tube with chemicals to keep it alive until they can grow it out and look at it under the microscope to see if she is dealing with one of these infections. I would definitely check with your childs doctors on testing her for this, because this definitely could be what is going on with her.
The other thing to look into is to see a neurologist who knows something about tethered cord. so, tethered cord is birth defect where the spinal cord is too short so when your daughter begins to exercise in any form she can begins to suffer with pain and neuro problems in her pelvic area and even down into her legs. They can easily check this by doing an MRI of her spine and measuring how far down the spinal cord is coming and if it is free to move around and not being impinged to one side.
Finally, if all of these things are fine then the you would need to work with a vulvodynia specialist to help her deal with the pelvic floor problems which cause the vulvodynia. It can take quite a few months of therapy and even some kinds of meds before she begins to feels some relief.
I hope this helps and your daughter begins to feel better. My heart goes out to you
I need help desperately! My Vulvadynia and Vaginism has been going on since I was 26. I’m 42 now and I’ve never been able to have intercourse. It burns constantly and urinating is the worst! It burns for probably 3-4 hours after I urinate, but never really stops. I have interstitial cystitis and Mayo said there may be a connection. I’ve done all the creams, pt, sitz baths, and as a last resort, had the skin removed surgically. I have never been in so much pain in my life as I was in that surgery. Someone told me about Dr. Fowler in Arizona that you can talk over the phone and he sends special soaps and creams. It healed a friend of mine. I can’t live with this anymore. Thank you.
Hi Lisa, I am so very sorry that you have been suffering like this for so long, my heart truly goes out to you. So, first I am not sure what all treatments you have been through. I know the few you have listed here but there are many more treatments that have higher success rates then what you have listed here, although I have never heard of them removing the skin in cases like this. That not only sounds painfully horrific but technically it should have exacerbated the situation, since a procedure like that would ultimately cause more trauma and pain to the area and both of those things ARE SOME OF THE LEADING CAUSES OF VULVODYNIA! So, I don’t know why any doctor would offer a procedure like that for this condition. Let me just state here that most well trained Gyne’s have been taught that when it comes to women with vulvodynia you want to cause as little trauma to the area as possible, meaning you don’t even do biopsies of the area unless absolutely necessary. You also should be using only fingers to examine and not a speculum whenever possible. So, this surgery was way out of bounds as a treatment for vulvodynia. Secondly, the burning with and after urination as well as IC are almost always seen with vulvodynia and that is because of two things. First, is that the urethra opening sits right in the vagina, so if the vagina is inflamed, the urethra will also be inflamed, and that will cause burning with urination and even afterwards. It will also make you feel as though you have to pee constantly and as if you have not fully peed when going. It can give the symptoms of UTI when you don’t actually have one. Second, thing is the nerves that innervate the bladder are the same nerves that innervate the vagina and even the colon. So, when someone suffers from vulvodynia, quite often they will also suffer from IC and even IBS of the colon, they go hand in hand due to the nerves that innervate the pelvic region. Let me also just state here that if vulvodynia is the first pain syndrome, quite often if it is diagnosed early on and treated effectively it can ward off the bladder and colon from also developing neurogenic and functional pain syndromes. The same holds true the other way, so if a person develops one of the neurogenic and functional pain syndromes, ,like vulvodynia and they are not diagnosed or treated correctly as soon as possible the nerves that innervate that area will begin to effect the nerve branches that feed the bladder and colon, so in time that person will develop these other conditions as well.
So, I don’t know if you have actually been to a pelvic pain clinic or if you have just been being treated by Gyne’s all this time, but if you have not been to a pelvic pain clinic, then I would suggest that you have your doctors refer you to one as soon as possible. Now I say this because Gyne’s are NOT specifically trained in treating pelvic pain conditions like vulvodynia, they may know about it and they may offer some creams or God forbid the surgery you under went (which again should never have been attempted with vulvodynia), but they truly are unaware of all the modalities that are used to treat this condition or even how this condition (vulvodynia) can spread to other areas and organs within the pelvic region and create other neurogenic and functional pain syndromes.
So, when you see a doctor who specializes in Vulvodynia as well as a pelvic pain therapist, they will examine you in very specific ways to help them figure out exactly where you problem lies in the vagina. So, they will check to see if there are specific areas of the vagina and they will also look at your lower back region and examine if your hips are in alinement, all of these things gives them a better idea on what may be causing your vulvodynia and with that information they order some more tests, such as blood work to look at your hormone levels as well as a CT or MRI to look at the vertbra’s and discs of the lower back which can impinge on the peudendal nerve that feeds all the nerves within the pelvic region. Once they have all this information they will try to set out a treatment plan that may include several different modalities, like pelvic floor physical therapy, hormone supplements, nerve reducing drugs like Amitriptyline or lyrica, certain exercises that strengthen and stretch the pelvic floor and supporting muscles and specialized diets to reduce your oxalate intake. Also because it has been so long since you have had intercourse they are going to need to do vaginal dilators to stretch the now atrophied vaginal muscles and walls. They can try any number of these things or even just one at a time. They will then watch to see if any of them begin to help and if not they will add in more of them or move on to more invasive therapies, such injections of an anesthetic and steroid or even botox to paralyze the nerves from sending messages to the spinal cord and then up to the pain center in the brain, this is also highly used in the treatment of IC. There are also spinal cord stimulators that can be either worn on the outside of the body in a little pack or placed just under the skin to send mixed signals to the spinal cord and pain center of the brain, so that the brain does not recognize the pain signals coming from those nerves.
Now depending on the reason for your vulvodynia they may find that your peudendal nerve is impinged in the back, which then they would correct that through surgery to release it. They may also find that you have what is known as tethered cord, where your spinal cord is to short or the phylum that surrounds it is to thick, therefore causing a “pulling” effect on the peundendal nerve and again this would need surgery to release it.
Now when they examine you they may also find that you have a history of other functional pain syndromes besides vulvodynia and IC, such as IBS, migraine headaches, fibromyalgia, chronic fatigue syndrome, painful periods and or heavy periods, ect.. This may lead them to a diagnosis of central sensitization syndrome, which also is quite often associated with vulvodynia and IC. In these cases they will still try to treat you with many of the modalities I listed above but will also have you under go cognitive behavioral therapy as well. This is a specific therapy that tries to retrain the brains pain center from over reacting to pain signals. It does help in many cases as an add form of treatment with other therapies. Let me also just say that people who often suffer with central sensitization syndrome have had some kind of spinal cord or brain injury, even if they do not know it, like from a serious fall or a car whiplash. They are also finding out now that many of these people with central sensitization syndrome also have tethered cord, which is a problem that originates at birth but often times is not a problem until the person grows into adulthood or experiences an injury to the spine or brain. So, this is something I would highly encourage you to check out and for a tethered cord diagnosis, I would also say that you need to find a doctor experienced in it, because many are not and will not realize that the phylum is to thick leading you to have a tethered cord and many do not know to do the millimeter measurements needed to diagnose tethered cord.
Finally, there are some other therapies that are now becoming mainstream like the use of medical marijuana, either smoked or even in a cream base that is then put into the vagina. I have heard of a lot of women gaining substantial relief from this therapy. However, with as far a long as you are in this pain syndrome, you will still need this form of therapy in adjunction to the other modalities I listed. I really do not think with as long as you have had this going on that any one form of treatment is going to be your answer. You see the longer you live with this more “ingrained” the nerves and brain become to the pain. Meaning that the brain becomes rewired to expect this pain even with least amount of pressure applied to the area and can even reach a point of just chronic pain whether the area is touched or not. In cases like this it usually takes a multiple modalities to lower that pain threshold and it definitely will require cognitive behavioral therapy to try and rewire the brain again. Now even with all this being said, I want to be brutally honest with you and say that because of how long this has been going on with you, you MAY never reach a point of being completely pain free, unless this is truly from a tethered cord or an impinged nerve in the spine. However, with the right treatment over time you can reduce that pain level down significantly, even to the point that you can enjoy intercourse again. So, I don’t want you to loose hope and please never give up, they are finding out more and more things as time goes on and I can tell you that even the worst vulvodynia cases out there do find treatment and regain their lives again, including sexual intimacy.
So, If your doctor does not know of a pelvic pain clinic in or around your area, then you can go to the National Vulvodynia Pain syndrome web site where they have a list of doctors in each state that treat this condition.
I truly hope this helps you and in case you have more questions or just want or need someone to talk to about this I will send you an email with my phone number so you can call me anytime. I wish you the best
has any research been done on a link between the Gardasil HPV vaccine and Vulvodynia? i regret having my daughter get that vaccine as it was totally unnecessary and after the first injection i had read some information about it that really concerned me (of course all the info sent home by public health, which was provided by the drug company, gave glowing reviews and made it sound life or death if they didn’t get the vaccine…..the drug company getting public health and all the schools on board made them millions) and decided we shouldn’t continue with the vaccine so i told her to tell the public health nurse that she wasn’t to get the next injection and i even gave her a note but the nurse told her she “had to get it” since she had the first dose and forced her to take it. i probably should have sued them. you mention there is a link between testing positive for HPV and vulvodynia but i just wonder if there could be a link between the vaccine as well. i know the drug company would try to suppress this link, if discovered, but please pass this on to any researchers to look into. i am interested to hear what others think about this. thank you
Hi Concerned Mother, I never came across any studies or research papers on a link between the Gardisil vaccine and vulvodynia. However, last night after reading your post I decided to go up and look to see if there was any, but could not find any linking the two together. So, I decided to look at the vaccine itself to find out if it was a live vaccine or not. I did find that the vaccine was NOT a live one, meaning the main part of the vaccine which is used to prevent the HPV virus is a synthetic mimic of the actual virus, so this means it is NOT an injection with a small amount of the live HPV virus. Then I went and looked at the physician’s information on all the possible side effects that have been seen and reported with this vaccine and again found no evidence or mention of vulvodynia and that even included the after market reporting. The only thing I did find was that there have been reports of Pelvic Inflammatory disease reported with this vaccine (besides all the other very serious systemic side effects). Now Pelvic Inflammatory Disease (PID) is completely different than Vuvlodynia, however if a person suffered the side effect of PID , they would be put at a much higher risk of developing Vulvodynia.
So, let me explain the HPV connection with vulvodynia and then I can explain why someone would probably not develop vulvodynia from this vaccine. You see, the virus itself (when you contract the actual HPV virus) does not ever leave the body, it goes into hybernation, much like many other viruses (herpes, EBV, CMV, ect..) These viruses hybernate in the persons tissues just waiting for the immune system to break down and allow it to come back out. Now with the HPV virus because it effects the tissues of the vagina and surrounding areas, it often sits deep within these tissues and around the delicate nerves that innervate these tissues. Each HPV virus cell contains a certain protein that sits on top of them. It is this protein that has been shown in studies to attach itself to the nerve endings within and around the vagina. This protein then basically irritates the nerve endings, therefore causing the vaginal pain known as vulvodynia.
Now, the HPV vaccine is a “dead” vaccine, meaning it is NOT Live, so it is not using the actual virus to stimulate the immune system into building a defense against the virus. This also means that the synthetic mimic of the HPV virus does NOT contain the actual DNA or protein that sits on the actual HPV cell, so it is not going to sit within the tissues, thereby attaching and negatively effecting the nerves that innervate the tissues. This means it does not have the ability to act on the body like the actual virus, therefore not setting off vulvodynia. So, this is probably why there are no known cases of this vaccine causing vulvodynia and probably why there are no studies speaking of it or on it.
Now, I know this vaccine has a history of damaging large populations of young girls and women who have gotten it, my daughter included, but vulvodynia is not one of the symptoms associated with it. However, I will tell you that when I looked up the actual ingredients of the vaccine, there is no wonder why so many are having problems with it. Besides the fact that you are being injected with a synthetic mimicked version of the virus, which is a foreign entity to the body and that alone can stimulate the immune system into attacking it and the body itself, but also many of the other ingredients are quite toxic and were never meant to be put into the human body. So, many of the other ingredients can also create a negative immune response and one that does not shut off, leaving the person to suffer with all kinds of autoimmune problems. Some of the other ingredients are also ones that if gotten into the muscular skeletal system could potentially set off muscular pain or illnesses like Fibromyalgia. So, there are a lot of reasons for your daughters response to this vaccine and I am sorry that she is also suffering with these problems, but vulvodynia did not come directly from the vaccine. Now let me just say that vulvodynia can often be set off by other immune illnesses within the body. Illnesses like Fibromyalgia as well as many of the autoimmune diseases, like RA or Lupus, ect… So, if your daughter is also suffering with vulvodynia now, even though it was not directly caused by the vaccine it could have been indirectly caused by the other systemic bodily illnesses that were caused by the vaccine. However, the way side effects are reported on drugs, it can only be listed or studied if it was a direct cause of something taken or used, but it cannot be listed, studied or connected as a side effect if it was indirectly caused by whatever was taken or used, such as the vaccine in this case.
Well, I hope this answers your questions and I hope that your daughter finds some kind of relief for her all of her problems now. Even though she may not have gotten vulvodynia from the vaccine, the treatments listed in this article as well as all the information should hopefully help you to help her find some kind of treatment at least for the vulvodynia. I wish you both the best
I have suffered with Vulvodynia for 20 years. Luckily my ob/gyn had read an article about it and got me to the only specialist in Boston. That being said I have done everything, everything medication , injections, pt, exercises, creams. marijuana etc. I just finished radiation for uterine cancer and my pain has exploded. My life doesn’t exist without this constant pain. You cannot overstate the mental battles involved. Constantly looking for answers is mentally and psychologically exhausting. Please keep up your work and making all the information available. I pray for answers and relief in my lifetime. Thank you!
I am so sorry to hear about your aweful battle with this horrible illness. I know you said you have done injections but i wonder if you have tried botox injections which are used in the most extreme protracted cases. Botox injections have a high success rate in cases like yours, if you have not tried this i would suggest bringing this up with your doctors. There are not a lot of places that do it, but usually university vulvar pain clinics are experienced in it, so you may have to travel but it may very well be worth your trip and time. I hope you find some relief.
Thank you for the Botox suggestion. I’ve had trigger point injections coupled with pt but never Botox. I will look into it. I’ve also not heard of magnetic dilators. They gave me 2 dilatory when I completed radiation but using them makes the pain worse. Do you think using magnetic ones would be any different?
Who is the specialist in Boston?
Kathy, I do not know specific doctors in each state that treat this condition, however, you can always talk to your Gyne, because they usually know of the nearest vulvar pain clinic and or vulvodynia specialists. If they are unable to help you find one you can go to the National vulvodynia Pain website where they also have lists of clinics and doctors in each state that treat this condition. I hope this helps you
Fantastic article
Thank you for this amazing article. Vuva Magnetic Dilators are incorporated into Pelvic Floor Pt for Vulvodynia and work well.
Tara, thank you for the kind words and your added input. I hope this article and women like you give some hope and maybe some alternative therapies to other women out there suffering. Thank you