Iodine is an essential element required for the propagation of chemical reactions that are needed to create the thyroid hormones Thyroxine (T4) and Triiodothyronine (T3). This process can be termed “Organification” whereby an inorganic molecule (iodine) is implemented in organic molecules (thyroglobulin protein). The organification process results in the production of these extremely important hormones. Any reduction of thyroid hormones, commonly through reduced iodine intake, will result in the debilitating symptoms of hypothyroidism. Unfortunately, iodine deficiency or insufficiency disorders affect around two billion people worldwide. In fact, iodine deficiency is considered to be the single greatest cause of preventable brain damage and mental retardation in children. The latter, known as congenital hypothyroidism, occurs during early childhood and results in stunted mental and physical development due to low iodine intake.
Iodine deficiency, however, can affect processes outside of thyroid hormones when the extrathyroidal action of inorganic iodine is disrupted. Extrathyroidal refers to iodine-mediated processes outside of thyroid-mediated organification (T4/T3) and is currently being more appreciated in the scientific and medical communities. The focus on thyroid hormones, understandably, has overshadowed scientific investigations regarding iodine’s role in extrathyroidal processes. As we will explore below, it turns out that other very important non-thyroid cells express receptors to transport iodine into the cell. These receptors can be regulated by the body in a similar fashion to the thyroid glands. That is, the body can increase them or reduce them (i.e. on/off switches) depending on the need.  Some of the functions of extrathyroidal iodine have been effectively implemented clinically in cancer therapy.
Some of the functions of extrathyroidal iodine have been effectively implemented clinically in cancer therapy.
Technical Note on Inorganic Iodine: The term iodine refers to the molecular state of iodine (I2) where two iodine atoms are bound together. The term iodide refers to ionic iodine which, similar to salts (i.e. sodium chloride), it can be found ionically bound to sodium or potassium (i.e. potassium iodide, sodium iodide).
Organification of Iodine Atoms
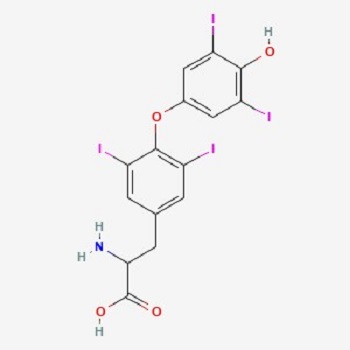
It is known that to make thyroid hormones (T4/T3) the body requires a sufficient supply of iodine. What is important to understand about this statement is that iodine is not just acting as an enzyme cofactor, but it is actually a part of the hormone. Thyroxine (T4) is 65% iodine by weight due to the relatively larger mass of the iodine atom (see PubChem image).
Briefly, the thyroid cells express a receptor called Sodium Iodide Symporter (NIS) which allows iodide to get into thyroid follicular cells from the plasma. The iodide molecule then moves into another compartment called thyroid colloid/lumen by another receptor named PENDRIN. From there it gets oxidized, from iodide to iodine, by thyroid peroxidase (TPO). The oxidized iodine finds a place in a protein named Thyroglobulin (TG) where all of the thyroid hormones are being built. There is a plethora of them on TG which include (T1, T2, T3, and T4). In this case, T4 refers to four iodine atoms present, while T3 refers to three iodine atoms.
Further reactions occur within TG allowing T4 and T3 to leave the thyroid. Here, 80% of the hormone mix is T4. Even though the thyroid glands produce mostly T4, T3 is the more active hormone and is produced from within other cells of the body such as the liver, kidneys, as well as immune cells. This is done by special enzymes called deiodinases that can convert thyroid hormones to multiple forms. In the end, T4 and T3 affect the metabolic processes of cells, which include thermogenesis, gluconeogenesis, glycogenolysis, and protein metabolism.
All of this comprises the hormone/organification process of iodine within the thyroid. Now let us look at the role of iodine in the rest of the body.
Iodine as an Antiseptic
Iodine is one of the best-known antiseptic agents with the least toxicity to human cells. When the term iodine is mentioned many, especially in the medical community, think of antiseptic or wound cleaning utility of iodine such as Povidone-Iodine. Iodine is used in such a manner because of its direct killing effects on bacteria. An example of this would be disinfecting a bucket of water or small wounds. The mechanisms of direct killing also happen within the body and include interference with the electron transport chain in bacteria, which human cells can better defend against.
Next, iodide can enter human cells by the specific transporters NIS and PENDRIN. In this case, the first direct mechanism occurs when the iodide form is converted into bactericidal molecular iodine through the actions of hydrogen peroxide with potential help of copper, as well as enzymes such as TPO and Myeloperoxidase. In this way, iodine is able to kill infections in localized areas (infection sites).
Iodine and Neutrophils
The second mechanism is semi-direct. Here, immune cells such as the neutrophils pull iodine into special cellular compartments called the phagosomes that are choke-full of hydrogen peroxide ready to convert iodide into iodine. This process is used by neutrophils to eventually make a bacterial-toxic compound called hypoiodite. Hypoiodite is even more bacterial toxic than hypochlorous Acid (active disinfectant component of bleach). Hypoiodite is used to “iodinate” bacterial cell walls. Interestingly, neutrophils also make a ton of hypochlorous acid naturally using chlorine atoms in a similar way to iodine. Therefore the neutrophils are given two halogen options (chloride and iodide) to kill microorganisms. Neutrophils will take either chlorine and make hypochlorite (bleach) or iodine and make an even more effective substance, hypoiodite. Chlorine is more abundant so cells typically “bleach” out bacteria or fungus.
Iodine to Treat Infection
Clinical Utility of Iodine in Treating Sinusitis: There have been recommendations by persons such as Dave Asprey (founder of BulletProof) for the use of iodine in treating acute or chronic sinus conditions. These recommendations make sense from what we have discussed above. However, more specifically, studies have shown the effective role of iodine in treating infected human sinus tissue. In this case, patients with chronic sinusitis were examined and were found to have a variety of microorganisms (Staphylococcus aureus and Pseudomonas bacteria & Yeast). Infected sites were extracted during surgery from the ethmoid region and then were exposed to potassium iodide, iodine tincture, or ethyl alcohol to control for the alcohol in the tincture. They used the Baclight assay which allows visualization of intact vs broken membranes of microorganisms via fluorescent microscopy. The findings were as follows:
- Iodine kills microbial pathogens even if they are within a biofilm.
- Treating for 10 minutes had similar effects as 30 minutes.
- Iodine tincture had slightly more destroying power than potassium iodide (SSKI).
The limitation here is that this study was done in vitro (in a laboratory setting), but nevertheless, it used human infected nasal tissue post-surgery. This, with the plethora of anecdotal stories from people who use iodine in this context, supports the importance of iodine in treating sinusitis.
Clinical Utility of Iodine in inactivating SARS CoV: Studies have shown that the direct effects of iodine apply to Coronaviruses. For example, gargling with povidone-iodine for only 15 seconds resulted in inactivating MERS-CoV and SARS-CoV. It is thought that the inactivation was due to inhibition of viral protein synthesis and alteration of the viral membrane. Because of this, it is almost certain that iodine would have a similar effect on the recent SARS-CoV2 virions. Some other researchers recommended the combination of Zinc, DMSO, and Iodide for the treatment of SARS-CoV2 infections and for boosting immune functions.
Iodine Promotes the Function of Human Immune Cells
There is yet a third iodine-mediated mechanism that the body uses to get rid of pathogens. That is, in addition to the direct mechanisms above, iodine can enter immune cells and activate gene transcription. Before addressing this aspect of iodine function, let us first briefly look at a study from the 1980s by Marani et al that alluded to the role of iodine and immune cells.
The study looked specifically at a group of Italian school-aged children in an area endemic of goiters. Out of 607 children, 48% had goiters despite many having normal thyroid values (TSH, fT3, fT4) with no apparent autoimmune reactions to thyroid peroxidase or thyroglobulin. The immune system of these children had deficient “delayed immune responses” as measured by skin testing – in essence, they assessed the adaptive immune response (T cells). It is important to note that some of the school children who were deficient in iodine also had reduced immune responses despite normal thyroid hormone levels. The latter statement is critical which demonstrates that just because your thyroid glands look normal on a blood test, does not equate to iodine sufficiency within the body. This is an important point since it is not common knowledge that inorganic iodine itself is important for cell function (outside of its role in thyroid hormones). For the treatment arm of the study, 215 children were given Lugol’s iodine (a mix of iodine and iodide) at a dose of 2 mg/week for eight months and were compared to controls not given iodine. After eight months, the children who received iodine had a marked restoration of immune responses with the same test compared to the kids who did not receive iodine.
The question stemming from this is how was iodine affecting immune cells? There were not too many studies that followed Marani et al and looked at specific mechanisms of inorganic iodine within immune cells, however, a recent study from our laboratory in 2017 showed some of what iodine is doing. In our study, immune cells were given iodine as sodium iodide or Lugol’s solution and then were assessed for activation at the protein and genetic level (ribonucleic acid [RNA] sequencing experiments). It was found that iodine “energizes” these cells by making them alter their genetic signature (RNA), which then promotes the release of proteins that are very important for immune function, termed cytokines. Within these cytokines, there is a group called chemokines. Chemokines allow immune cells to move better through the body, to kill tumor cells, and to fight infections. Overall, this has large implications for the cells interacting with iodine in the gut and other places in the body like in the blood, liver, thymus, and other cells. Importantly, no alteration of thyroid hormones were observed between iodine treated and non-treated immune cells. Therefore, these effects seen were directly caused by inorganic iodine and not by thyroid hormones.
Immune System Studies within Animals: Another recent study on dairy cows confirmed our laboratory’s results in human cells. The study demonstrated that when dairy cows were given iodine, significant changes were detected in their genomic transcriptional activity (RNA). The authors show that up to 525 genes were altered when cows were given iodine! Some of the significant gene changes were Fc Receptors – these receptors are located in phagocytic immune cells that can “eat up” bacteria. Iodine also caused an increase in genes that activate immune B cells – these are the cells that produce antibodies and protect against a variety of infections such as SARS-CoV2. Antibodies mark cells and foreign invaders for attack and destruction. Again, the increase in immunity was not due to enhanced thyroid hormone synthesis. Therefore, iodine can control specific gene expression in these dairy cows.
For a more in-depth discussion of iodine and different types of immune cells, the reader is referred to this manuscript.
Utility of Iodine in Cancer Treatment
There is no doubt that without an effective immune response, one would be susceptible to a variety of cancers. We’ve already seen how iodine can improve the immune response towards more activity, trafficking, and killing mechanisms. These mechanisms apply to both pathogens and cancer cells that can be located by specialized immune cells. We can then hypothesize that a deficiency of iodine will reduce the immune response (as observed in the Italian children’s study), and thence substantially increase the chances of cancer development and/or progression.
Clinical Utility of Iodine in Breast Cancer Treatment, Study 1: Moreno-Vega et al showed in 2019 that iodine can be very effective in treating breast cancer. They used 60 women who were in early (stage II) and advanced (stage III) stages of breast cancer and then gave them 5 mg/day of iodine along with placebo controls. They relate in their conclusion:
I2-treated tumors exhibit less invasive potential, and significant increases in apoptosis, estrogen receptor expression, and immune cell infiltration. Transcriptomic analysis indicated activation of the antitumoral immune response.
They also found that the five-year disease-free survival rate was a lot higher in patients receiving the iodine. Here we see that the mechanisms discussed above are at play in real patients as follows:
- The immune cells were activated and were able to traffic better to tumor tissue!
- Changes within the tumor cells were seen indicating that inorganic iodine directly affected the cancer cells.
Clinical Utility of Iodine in Breast Cancer Treatment, Study 2: Mendieta et al showed in 2019 that “I2 decreases the invasive potential of a triple-negative basal cancer cell line, and under in vivo conditions the oral supplement of this halogen activates the antitumor immune response”. In other words, iodine inhibited breast cancer metastasis.
Clinical Utility of Iodine in Breast Cancer Treatment Study 3: Another study coinciding with the writing of this discussion (September 2021) showed that I2 induced the immune response by affecting the methylation status in specific sites of the genome [more information on methylation on this blog post]. Some of these genes are cytokine genes such as Interferon Gamma which acts in the anti-tumor immune response. In essence, Interferon Gamma gene regions become “de-methylated” which makes the gene more active in the cell. They also showed increased infiltration (increase) of immune cells named macrophages. These cells are important because they collect information from tumor and infection sites and then relay them to the killer immune cells (T cells).
Other studies have shown similar results using shock wave therapy with iodine. Additionally, there are now clinical trials to further look at these great direct and indirect anti-tumor effects of iodine. There is no doubt from these studies that iodine carries strong anti-tumor properties.
Role of Inorganic Iodine with Regards to Fertility
Analysis of the US population by the National Health and Nutrition Examination Survey (NHANES) has shown that about 35% and 38% of women of childbearing age and pregnant women, respectively, had less than 100 µg/L of urinary iodine levels. This is below the current recommended reference range and demonstrates iodine deficiency. Importantly, approximately 58% of women of the childbearing age had less than 150 µg/L of urinary iodine. The latter number is below RDA for pregnant or lactating women. This should be of major concern for public health given the effects of an iodine deficiency on human health such as mental retardation, infertility, and reproductive failures. This is in part due to lowered metabolic rates from the low production of critical thyroid hormones.
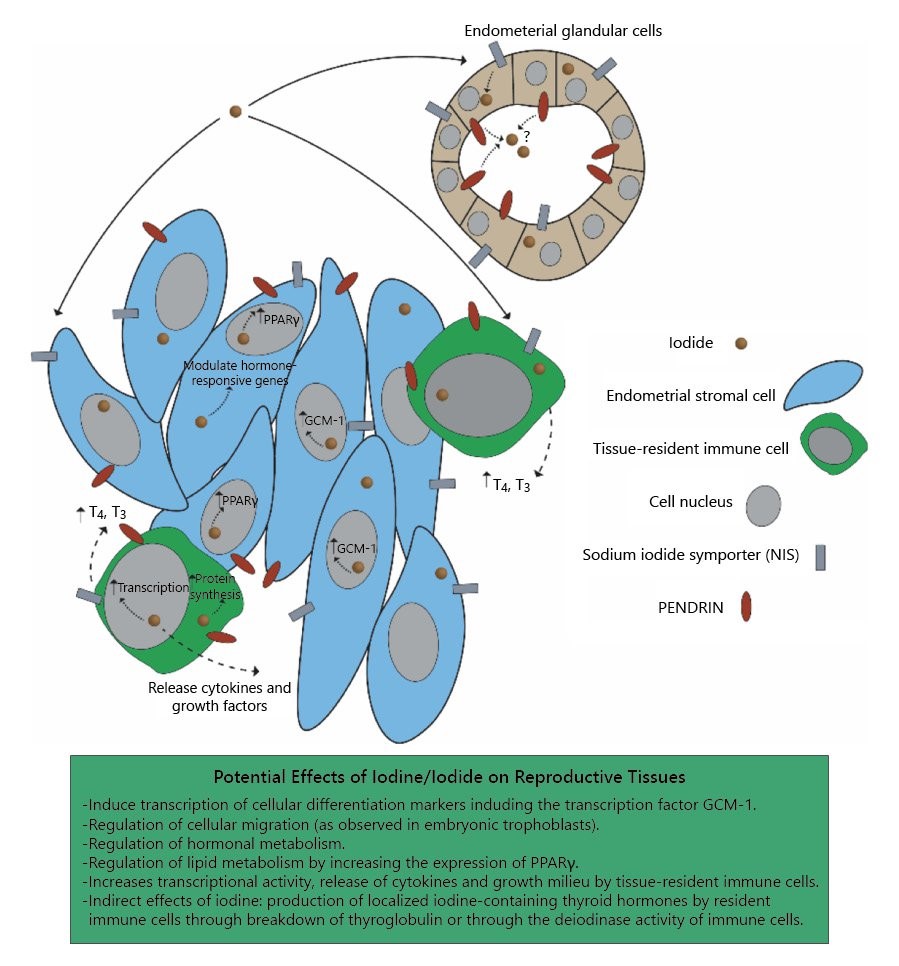
What about extrathyroidal iodine? Similar to immune cells, recent studies from our laboratory (2020) have also shown that the human endometrium can express iodine receptors. This study was performed with the assistance of Dr. David Brownstein who is an iodine expert. Briefly, the study shows gene analysis data (RNA Sequencing) that demonstrate the possibility of localized iodine deficiency in women with reproductive pregnancy loss or implantation failures compared to controls. We hypothesized from these findings that inorganic iodine (i.e. sodium iodide, potassium iodide, molecular iodine obtained from food) is needed for proper cellular function in reproductive tissues, and that iodide transporters [receptors] may potentially be used as a marker for infertility or for probing potential localized iodine deficiency that may not present in a typical thyroid panel analysis.
Can Non-thyroid Human Cells Produce Thyroid Hormones by using Iodine?
One of the questions inquired by the 2017 immune cell study above was if any other human organ or cells can produce thyroid hormones. The classical view is that only the thyroid can do this, and indeed the thyroid bears the weight of making these hormones. However, it turns out that immune cells can perform very similar functions to the thyroid. The same 2017 study showed that human immune cells could uptake the Thyroglobulin protein and then produce from it thyroxine (T4) and triiodothyronine (T3). These cells can also potentially make thyroglobulin and iodinate it using inorganic iodine – although organification of thyroglobulin by iodine has not yet been clearly shown experimentally outside of the thyroid. Nevertheless, the study shows that your thyroid is not the only place where thyroid hormones can be made! In addition, the immune cells seem to be very good at converting T4 to T3 and therefore can help in making you feel more energized.
Recommended Dose of Iodine
The subject of daily recommended iodine intake is extremely controversial even within functional medicine groups. Part of this controversy is due to the fact that a small population can respond negatively to high-dose (> 12-100 mg) iodine supplementation by amplifying autoimmune thyroiditis (increased thyroid antibodies). While this is true in some cases, it is not common and the missing link for that group is probably, in part, deficient antioxidant defenses. This includes reduced levels of selenium, glutathione, and copper. Anytime iodine is ingested, the thyroid ramps up hydrogen peroxide production and reactive oxygen species. If there are no antioxidant defenses, well then the person is left defenseless against thyroid injury and autoimmune antibody production.
One faction of the debate that is not as controversial with a better consensus, is that we certainly need to increase the minimum iodine RDA from 150 µg to around 0.5-3 mg (500-3000 µg). This is because we are understanding more that other body tissues need to utilize iodine as discussed above and that other non-thyroid tissues store iodine. Additionally, therapeutic studies discussed above-used doses in this range and up to 5000 µg. Some others take the middle road and recommend at least 1000 µg. Other very well-regarded physicians who are experts in treating patients with iodine go as high as 50-100 mg per day (50000-100000 µg). Regardless, with any supplementation, one must consider advice from qualified medical practitioners to avoid negative unnecessary side effects.
Conclusion and Future Developments
We can appreciate from recent studies that the human genome is set to respond to iodine and at the same time utilize it for fighting infections. When one is sufficiently replete with iodine, they are able to destroy microorganisms directly but also ramp up multiple indirect and direct mechanisms by the intricate network of the human immune system. Overall, from the above discussion we can conclude the following:
- Iodine can directly kill microorganisms such as bacteria, viruses, and yeast by interfering with their electron transport chain, protein synthesis, or cell membrane.
- The immune system can utilize iodine in powerful compounds such as hypoiodite to kill microorganisms.
- Iodine and iodide can enter immune cells and affect gene transcription and the function of immune cells. These effects have been shown to enhance the immune system in human cells as well as within large animals.
- Iodine has been used successfully to treat cancers. Part of its anti-tumor effects are both direct (on tumor cells) but by also activating the immune system.
- Some women with infertility or recurrent pregnancy loss seem to have low iodine levels in their reproductive tissue.
- Immune cells are able to produce thyroid hormones given the proper environment.
- “Normal” thyroid blood tests do not necessarily correlate with complete iodine body sufficiency.
Certainly more studies are underway to define the role of extrathyroidal iodine in all body compartments. For example, the author speculates that iodine is important for liver detoxification. This is because cell culture studies showed that iodine can increase levels of Cytochrome P450 enzymes which is likely to also occur in the liver in response to iodine replenishment. While it would be difficult to attain a complete review and consensus regarding the recommended daily doses of iodine, the research presented above suggests that we certainly need more than what is currently recommended.
Further Recommended Reading
Bilal MY, Dambaeva S, Kwak-Kim J, Gilman-Sachs A, Beaman KD. A Role for Iodide and Thyroglobulin in Modulating the Function of Human Immune Cells. Front Immunol. 2017 Nov 15;8:1573.
Bilal MY, Dambaeva S, Brownstein D, Kwak-Kim J, Gilman-Sachs A, Beaman KD. Iodide Transporters in the Endometrium: A Potential Diagnostic Marker for Women with Recurrent Pregnancy Failures. Med Princ Pract. 2020;29(5):412-421.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Feature image created using Canva AI.
This article was published originally on September 20, 2021.






