In a previous piece, I discussed some of the problems that could occur when supplementing with a particularly potent form of thiamine called tetrahydrofurfuryl disulfide or TTFD. Specifically, we examined how TTFD can temporarily deplete glutathione (GSH) and increase the recycling requirements (using activated riboflavin and NADPH). I also provided some recommendations for how one might improve this initial processing of TTFD in cells. Following on from that, we will now look at the next phase of TTFD processing to help pinpoint some of the reasons why some people suffer negative reactions when beginning supplementation. In short, the clearance of TTFD breakdown products requires adequate methylation capacity and many individuals who are thiamine deficient have insufficient methylation.
From Glutathione to Methylation
Once TTFD has been reduced (or “broken apart”) by glutathione (GSH), it is further bound or conjugated with more GSH, likely using the enzyme glutathione-s-transferase. This reaction produces a conjugate called glutathione tetrahydrofurfuryl disulfide (GTFD).
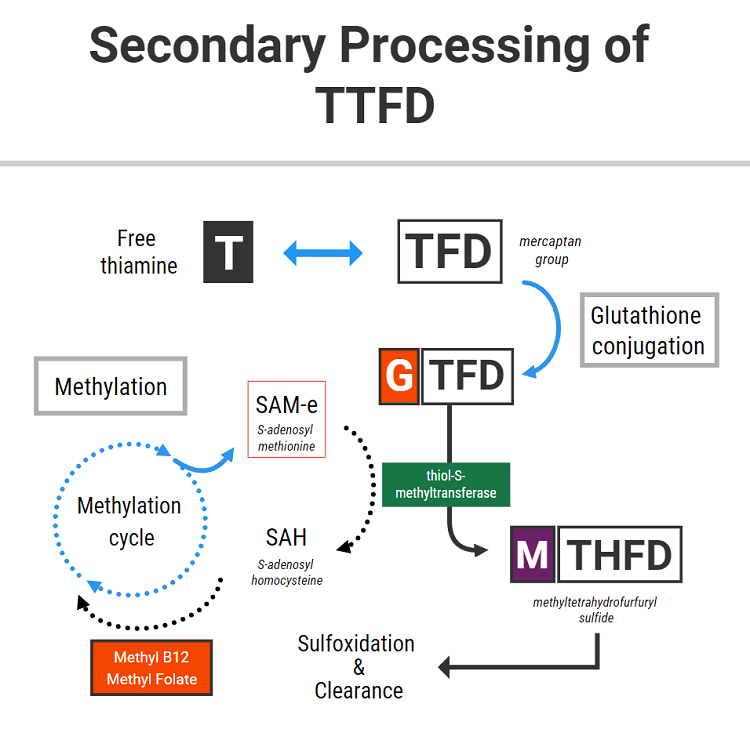
The above diagram shows that this GTFD conjugate then needs to be methylated. Methylation is the process by which a methyl group is attached to its structure from a donor molecule (a “methyl donor”). The major methyl donor in cells is called S-adenosyl methionine, commonly known as SAM-e.
SAM-e is generated through a biochemical cycle called the methylation cycle. Dietary protein provides amino acids, one of which is methionine. Through combining with ATP, methionine can be “activated” to generate SAM-e. SAM-e possesses a methyl group, which it then donates to a variety of different molecules via methyltransferase enzymes. In simple terms, attaching a methyl group to a molecule serves to change its function in some way.
After having donated its methyl group, SAM-e becomes SAH (S-adenosyl homocysteine) and later homocysteine. Homocysteine can either be recycled back to methionine with the use of multiple nutrients (including folate and vitamin B12), or alternative can be drawn down through the transsulfuration pathway to generate cysteine.
The newly recycled methionine can further serve as the source of more SAM-e, which continues to be utilized in methylation reactions. This is ideally how the process should work.
Methylation is involved in DNA base synthesis, gene expression, detoxification, neurotransmitter production/clearance, and many other processes. As SAM-e is the major cellular methyl donor, cells must maintain a consistent level of SAM-e to fulfill those functions.
Since methylation is required for the synthesis and clearances of neurotransmitters and maintaining neurochemical balance in the brain, it is thought that changes in methylation status can be responsible for the underlying neurochemical abnormalities present in various psychiatric disorders. For the above reasons, SAM-e has been used effectively as a fast-acting anti-depressant medication and is also useful as an anxiolytic agent in specific cases.
In the context of longstanding deficiencies in the nutrients required to maintain a healthy methylation cycle, a relative inability to recycle homocysteine can yield elevated levels of homocysteine and consequentially less SAM-e. And because SAM-e is the primary methyl donor in the cell, methylation (and by definition, all of the many processes which require methylation) can become compromised.
TTFD and SAM-e
The above information is relevant to this topic because the breakdown of TTFD requires adequate levels of SAM-e. Through the enzyme thiol-s-methyltransferase, SAM-e donates a methyl group to GTFD to generate methyl tetrahydrofurfuryl disulfide (MTHFD). MTHFD is then later funneled through the sulfoxidation pathway in the liver to be cleared primarily through the urine.
The nuts and bolts of this: TTFD metabolism can deplete SAM-e. A lack of SAM-e could potentially help to explain some of the following side effects which are common with this therapy – including insomnia, anxiety, agitation, restlessness, flat mood, fatigue, and/or mild depression.
Oftentimes, it is assumed that these symptoms are caused by an inability to process the sulfur content of the molecule, or are simply a manifestation of the “paradoxical reaction”. Sometimes it subsides within a few days or weeks, whereas other times it doesn’t. The reason for this, in some people at least, might relate to changes in methylation status.
Furthermore, by using up SAM-e, TTFD could also theoretically increase the requirement for some of the other nutrients involved in the methylation cycle. These might include the B complex vitamins, particularly folate, riboflavin, and vitamin B12.
Clinical Experience Suggests A Relationship Between Methylation and TTFD Response
And so, might this be one of the mechanisms by which TTFD therapy can go on to “unmask” an underlying folate/B12 deficiency in some people? Dr. Lonsdale has documented cases of folate deficiency being “unmasked” in some people after undertaking thiamine therapy. I have also seen this on several occasions, and I suspect in some cases, it might be somewhat related.
Secondly, a lack of SAM-e can then theoretically produce neurochemical changes which are potentially responsible for sudden feelings of anxiety or depression that some people tend to experience.
This would especially apply to those people who already have compromised methylation, or tend towards lower levels of SAM-e, folate, B12, or a combination of all three.
To conclude, this highlights the importance of B complex therapy in conjunction with TTFD, as well as monitoring nutritional status at regular intervals if experiencing negative symptoms or side effects from this nutrient. If you are one of the people who experience depression or anxiety from taking the TTFD form of thiamine, then you might want to try investigating methylation status, or experiment with methylfolate, methyl B12, betaine, or SAM-e.
We Need Your Help
More people than ever are reading Hormones Matter, a testament to the need for independent voices in health and medicine. We are not funded and accept limited advertising. Unlike many health sites, we don’t force you to purchase a subscription. We believe health information should be open to all. If you read Hormones Matter, and like it, please help support it. Contribute now.
Yes, I would like to support Hormones Matter.
Image by Michael Schwarzenberger from Pixabay.
This article was published originally on January 7, 2021.
















I have found that sunflower lecithin has a major impact on my energy, mood, motivation. I decided to try it because I read it helped support methylation and I believe it supports SAMe production. For me, it feels better/more natural than supplementing specifically SAMe. And it is cheap. It’s the way to go imo if you need support in this way. I have a slow COMT gene and I believe that’s in part why after long periods of drinking coffee I started feeling off (COMT determines how well your body clears stimulants). Sunflower lecithin has the capability of helping me sleep better while also giving me better energy during the day. Very interesting thing that most people are not aware of, and tend to supplement SAMe directly instead of this.
ENERGY UTILIZATION.
It is important to understand that thiamine STIMULATES energy production. Transmethylation CONSUMES energy. That is why they obviously need each other. The nearest analogy is that a car needs an engine AND a transmission.
Is there a methylated form of TTFD? I take 2 forms of thiamin, one being benfo and the other is included in B+ by Seeking Health/Ben Lynch.
I don’t know my methylation status, but am MTHFR a1298c. I apologize. My cog function is very impaired. Also, have been on an untold # of psych drugs for nearly 3 decades (originally Zoloft for mild fatigue, not anxiety or depression), still suffering GREATLY from a yearlong taper off of Pristiq in 2010-11.
*Would SAM-E provoke or exacerbate akathisia or other neurotoxicity from taking OR WITHDRAWING FROM these drugs?
Brain MRIs show degenerative, dementing process (diffuse lesions and frontotemporal atrophy).
I’m so overwhelmed and losing any desire to push on.
Thank you all for the work you do.
Thank you so much. I’ve know for awhile now that I have issues with both thiamine deficiency and undermethylation but haven’t been able to determine a protocol that manages to address both. I trust this will help a great deal. Thank you!
Thank you so much for this! As per the Walsh protocol, I am a classic histadelic but months of SAMe and supporting nutrients have failed to alleviate my symptoms sufficiently. I also have had great improvement at times from TTFD, magnesium and a full B complex in significant doses but I was never sure how to integrate the two protocols because they did seem to be linked but in a way that remained unclear to me. I appreciate your thorough elucidation so much.
Can we simply test for thiamine deficiency? Would an in range reading suggest thiamine deficiency is not the issue with some oxalate symptoms?
Thanks for the article Elliot. About 3-4 weeks after starting with TTFD, I was getting the side effects you mentioned (exhaustion, slight depression) just by alternating between 50 mg TTFD or a low dosage b-complex every morning. I was already taking magnesium every night as well. Upon closer examination I realized my b-complex didn’t have any Folic Acid or B12. I bought an activated b-complex with folate and methylcobalamin and that restored the subtle euphoric feeling I get from TTFD.
I am homozygous for C677T and other mutations in the methylation cycle. I am on 150 mg TTFD for the past 3 years. I have experienced the apathy type depression you mention. It is due to choline depletion. When the methylation cycle isn’t working it goes down the BHMT pathway and uses up choline. I took 2 g of trimethylglycine for a while and it worked to combat the depression. I don’t use that as often now, I take P5P (Active B6) as well as 300 mg of B2 a day.
If we compare the body to an automobile, the same principles apply. A car burns gasoline in an engine. Cells in the body burn glucose in mitochondria. Thiamine and its colleagues enable it to occur, just as a spark plug ignites gasoline in a car. In both the car and the body, energy is produced. In the car the energy produced in the engine is passed to the wheels through a transmission, a series of interlocking metal parts. In the body the energy is used to run the trans-methylation mechanism, a series of interlocking chemical reactions. For example, folate and B12 require ATP to be activated. An inadequate supply of ATP results in their inactivation. They then accumulate in the blood in an inactive form. That is why autism is predictable as an example of energy deficiency when the maternal blood during the pregnancy is found to have an elevation of folate and B12. Since thiamine deficiency is probably the commonest cause of energy failure this combination of circumstances strongly suggests that one of the causes of autism is thiamine deficiency.
Thank you for this information. I published my story on this site not long ago (Rapidly Deteriorating Health with Thiamine Deficiency). I have severe beriberi, and my struggle is ongoing. I’ve experienced a similar reaction to TTFD as what’s described by your client. I had initial astounding results of brain clarity that after several weeks shifted into severe anxiety, feelings of toxicity, and eventually sensations of brain injury with each dose. I recently dropped the 600 mg of TTFD I was taking altogether after the cognitive impairment grew so intense it felt like hypoxia (sensation of being semi-conscious or asphyxiation, altered sensory processing, extreme dizziness, and difficulty focusing, making decisions, and very poor short-term memory). After more than ten days now, I am still dealing with these symptoms to some extent, despite having immediately replaced TTFD with thiamine hydrochloride.
I tested TTFD with a biofeedback machine in the initial stages of using it with fantastic results. The machine said it was good for virtually all my organ systems; however, upon recent testing, it showed no benefit and a great deal of toxicity. Having listened to your videos about TTFD and reading your prior article on this website, I had some degree of understanding about the likelihood that my glutathione was depleted and that methylation issues and SAMe likely also played a role.
I’m not sure how to go about replenishing what TTFD depleted or how to restore my cognitive function, which was already compromised by beriberi. My B12 level is 702,173 pg/ml, and my folate is 241.3 ng/ml. These levels could quite possibly be toxic, and are likely related to my longstanding thiamine deficiency, rendering my cells unable to properly uptake these nutrients. Prior to learning thiamine deficiency and beriberi were the cause of the symptoms I developed in May 2020, I was self-administering B12 injections, thinking pernicious anemia may be a factor. That is certainly a contributing factor to the extremely high B12 blood level as well. Given that supplementing B12 and methylfolate definitely aren’t good options for me, do you have any guidance on prudent things to try?
One supplement that tested well for neurological functioning with the biofeedback machine is ornithine. Ornithine is commonly used to clear excess ammonia from the brain in detox protocols or in hepatic encephalopathy. In my recent experimentation, it did provide some relief from the sensations of cognitive impairment and anxiety. Do you have any experience with ornithine? I’m hesitant to use it regularly because my most recent kidney labs showed elevated creatinine (1.05) and low GFR (58), and ornithine is not recommended in kidney disease.
The kidney function decline is totally new in my lab work, and I wonder if the TTFD had a role to play. I was also supplementing benfotiamine along with TTFD, so it’s possible either one had an impact. I’m not sure what else would be a factor. I am 39, eat a paleo whole-food diet heavy in vegetables, and do not take any pharmaceuticals. I’ve wondered about the possibility of oxalates being an issue; however, when I asked the biofeedback machine, the answer is no.
I truly feel at the end of my ability to cope. These past eight months have been extraordinarily challenging, but after taking R-lipoic acid in early November and going rapidly downhill (subsequently learning my health problems were due to thiamine deficiency), life has been virtually unbearable. I’ve no doubt TTFD saved my life in the initial stages of taking it, but the benefits definitely disappeared after several weeks and contributed to more negative symptoms. Taking anything beyond thiamine hcl, magnesium, a b complex called B Minus (which contains no folate or B12), citicoline, and ubiquinol feels like playing Russian roulette. I can’t afford to make anything worse at this point, but I’m desperate for relief.
Any guidance would be deeply appreciated. Thank you.
Is there not anything you can do to improve your mental state?
Are you calm?
Therese, with all due respect to Dr. Lonsdale, I had a bad reaction to TTFD as well and I don’t think it has anything to do with glutathione depletion, etc.. It is an extremely bitter compound. EXTREMELY so.
The bitter taste is seen in TCM (Traditional Chinese Medicine) and also ayurvedic medicine as ‘drying’ and depleting yin (blood). You know, if you think about what we eat on average, bitter foods are in the minority. That’s for a reason. If you ate bitter greens all day, I guarantee you’d be very uncomfortable. I would stick with the thiamine HCL, or maybe try thiamine mononitrate.
Also ornithine has been a lifesaver for me. I haven’t read anything in any reputable journal with regards to harming kidney function. You might also consider dropping the B-Minus as b6 can cause a lot of neuropathy, even in small doses.
Lastly, are you getting enough carbohydrates? I know Elliot pushes a very low carb diet, but in order for thiamine to work, you need some carbs.
There’s a case study with an anorexic woman who was given thiamine, but developed hypothermia when she started eating less. Nothing helped until “the patient’s intake of sucrose was abruptly increased, and her body temperature normalized within seven days.”
She needed SUGAR to help the thiamine raise her body temp.
Lastly, are you getting enough protein? Edema is a hallmark not only of thiamine deficiency but of kwashiorkor — a.k.a. protein-calorie malnutrition. One needs methionine (especially) to reverse that.
Good luck.
I was also taken aback by how incredibly bitter allithiamine is, tastes like pure poison.
Is it really safe?
Hello Kelly,
Thanks for your reply. I’m still heavily struggling with cognitive function decline and feelings of brain injury. My diet contains a good balance of carbohydrate, fat, and protein. I eat a wide variety of quality protein from animal sources, nuts, and seeds, and also plenty of carbohydrates from fruit, berries, and yams, and sweet potatoes. The only foods I don’t eat are grains, dairy, and legumes.
Do you use Ornithine Aspartate? In what quantity and frequency do you use Ornithine?
B6 has tested well for me in biofeedback at 30 mg per day, so I feel comfortable using it. At this point, much of my nerve damage has actually healed. It is now the brain issues that are completely dominating and have destroyed my quality of life.
I’m sorry Therese — I didn’t see your reply until now. I hope you’re doing better these days.
I take ornithine mononitrate, and take 500mgs 3-4x per day. I’ve recently added citrulline, as that also helps lower ammonia. I was taking twice the amount of ornithine, but think it was dilating my blood vessels too much, hence the addition of citrulline.
The brain requires glucose for energy. Perhaps you’re getting too much fructose, which can lead to insulin resistance if one gets too much. That can cause cognitive issues as well. You might consider more starches, even maltodextrin, just to see if getting more glucose helps. Thiamine definitely helps one use glucose as noted in my earlier reply.
I’m not so sure I’d trust a biofeedback machine. I don’t mean anything personal as I used to go to some docs who used them as well. But keep in mind that that machine was the one that said the TTFD in 600mg doses was right for you…
Hi Therese, has any of this improved for you in the time since?