My life and health were turned upside down after my unwarranted hysterectomy. I touched on the internal and external anatomy changes in a previous article. I am going to go into more detail here on the effects of hysterectomy on the internal anatomy.
Female Anatomy
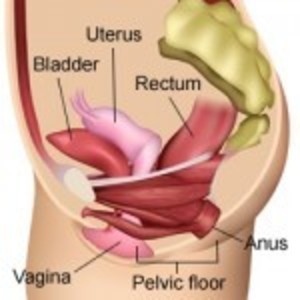
The uterus sits in the center of the pelvis held in place by four sets of ligaments. The uterus separates the bladder and the bowel and holds those organs in their rightful positions. Once the ligaments are severed and the uterus removed, the bladder and bowel drop down and, without the uterus to separate them, are now adjacent to each other. The nerves and blood vessels that are severed during hysterectomy may also alter the functions of pelvic organs. This female anatomy video explains the anatomical (and other) effects of hysterectomy.
What Every Woman Wants to Know about Hysterectomy
Pelvic Floor Disorders after Hysterectomy
What do medical studies say about the effects of these anatomical changes on the pelvic floor and organ function?
This 2014 U.S. study concluded that hysterectomy is one risk factor for developing pelvic floor disorders. The others are higher Body Mass Index (BMI) and greater parity. There are a number of studies that came to this same conclusion.
This large 31 year Swedish study concluded that hysterectomy, particularly vaginal hysterectomy, even in women with no vaginal births is associated with pelvic organ prolapse surgery. The number of vaginal births further increases this risk.
According to this large Swedish study, vaginal hysterectomy had a higher risk of surgery for pelvic organ prolapse or stress urinary incontinence than other modes of hysterectomy.
Of course, women who undergo pelvic organ prolapse surgery represent only a subset of those who suffer symptoms of bladder and/or bowel dysfunction.
Bladder Function after Hysterectomy
A number of studies have shown no short-term urinary adverse effects of hysterectomy. However, longer-term follow-up shows an increased risk. This large Swedish study over a 31 year period (1973 to 2003) showed a 2.4-fold risk of urinary stress incontinence surgery in women who had hysterectomies for benign conditions. This Danish study of women aged 40 to 60 years also showed a 2.4-fold risk of stress incontinence in women who had a hysterectomy. A small China study showed a 7.6% rate of pelvic organ prolapse and 67.4% rate of urinary incontinence 6 years post total hysterectomy.
A systematic review of 12 MEDLINE articles that used original data published over a 32 year period (January 1966 to December 1997) “was consistent with increased odds for incontinence in women with hysterectomy….Among women who were 60 years or older, summary odds ratio for urinary incontinence was increased by 60% but odds were not increased for women younger than 60 years.” Another review of this same data consistently found an increased risk of incontinence many years after hysterectomy. However, this study also concluded that “Oral estrogen replacement therapy seems to have little short-term clinical benefit in regard to incontinence and is associated consistently with increased risk of incontinence in women aged 60 years and older in epidemiologic studies.”
The latter statement begs the question “Is the association of oral estrogen and incontinence solely from the oral estrogen or could it be that it’s caused by hysterectomy that prompted the use of estrogen?”
Hysterectomized women of ALL ages were at increased odds for urge (1.9) and bothersome urge (2.6) urinary incontinence (but not stress incontinence) according to this Netherlands study of 1,626 women. This French study of 1,700 women also concluded that hysterectomy increases risk of urge, as well as stress, incontinence regardless of age.
In contrast, this analysis of studies done on urodynamics before and after hysterectomy concluded that “Hysterectomy for benign gynecological conditions does not adversely impact urodynamic outcomes nor does it increase the risk of adverse urinary symptoms and may even improve some urinary function.”
This small study compared incontinence / continence at 1 to 3 years post-hysterectomy and again at 4 to 6 years post-op. Interestingly, some women went from being continent to incontinent while others went from being incontinent to continent.
Why the conflicting results? There are a few things that come into play, the more obvious ones being study design and size as well as the follow-up period. Mostly, the results depend on the reason for the hysterectomy and whether a bladder suspension was done at the same time. Two common reasons for hysterectomy are fibroids and uterine prolapse. Both conditions can cause urinary symptoms such as frequent urination and incontinence. So symptoms may improve after hysterectomy and if the bladder was suspended at the time of hysterectomy (in the case of prolapse), that would also explain improvement.
Bowel Function after Hysterectomy
Some studies show that hysterectomy negatively affects bowel function. While this small and short-term 2004 study (comparing pre-operative to 6 and 12 months post-operative) concluded that vaginal hysterectomy does not increase incontinence or constipation, abdominal hysterectomy may increase risk “for developing mild to moderate anal incontinence postoperatively and this risk is increased by simultaneous bilateral salpingo-oopherectomy.” In contrast, this small 2007 study found that vaginal hysterectomy significantly increased anal incontinence at the three-year point and at one and three years for abdominal hysterectomy. However, there was “no significant rise in constipation symptoms or rectal emptying difficulties in either cohort through the follow-up.”
This contradicts this small case control study that showed significant short-term decreased bowel frequency and increased urinary frequency after hysterectomy. It also contradicts this larger Netherlands retrospective study in which 31% of women reported severe bowel function deterioration and 11% reported moderate bowel changes after hysterectomy. In the control group which consisted of women who underwent laparoscopic cholecystectomy, 9% reported “disturbed bowel function.”
Constipation, straining, lumpier stools, bloating, and feelings of incomplete evacuation were reported by women who had undergone hysterectomy in this small study.
Abdominal hysterectomy is associated with a significant risk of fecal incontinence and rectoanal intussusception according to this small retrospective study.
Post Hysterectomy Fistula
Hysterectomy increases risk of fistula as documented in the below excerpt from this article:
The uterus precludes fistula formation from the sigmoid colon to the urinary bladder.
As well as this excerpt from this article:
The most common types of fistula are colovesical and colovaginal, against which the uterus can act as an important protective factor.
Diverticulitis is a known risk factor for fistula formation. This large study looked at the risk of fistula formation in hysterectomized women with and without diverticulitis using data from women hysterectomized between 1973 and 2003. Women who had a hysterectomy but no diverticulitis had a 4-fold risk of fistula surgery compared to women who did not have a hysterectomy or diverticulitis. Women who had a hysterectomy and diverticulitis had a 25-fold risk of fistula surgery whereas non-hysterectomized women with diverticulitis had a 7-fold risk.
Vaginal Vault Prolapse
The International Continence Society defines vaginal vault prolapse as “descent of the vaginal cuff below a point that is 2 cm less than the total vaginal length above the plane of the hymen.” This Obstetrics and Gynecology International article states that “it is a common complication of vaginal hysterectomy with negative impact on women’s quality of life due to associated urinary, anorectal and sexual dysfunction.” The article cited above explains the mechanism for this common complication in section 2 titled “Anatomic Background.”
Table 3 in section 12 compares vaginal and abdominal corrective surgery outcomes using a 5 year follow-up. Vaginal had significantly higher post-operative incontinence and recurrence rates. The re-operation rate due to recurrence was 33% in the vaginal group versus 16% in the abdominal group.
Surgical mesh is used for many pelvic organ prolapse surgeries. And as shown by the TV ads, surgical mesh has high complication rates. It can cause infection and the mesh can protrude into the vagina leaving sharp edges having obvious negative effects on male partners. And removal of all traces of mesh may be impossible because tissue grows around the mesh.
Women who have not had a hysterectomy and have pelvic organ prolapse may choose to use a pessary instead of undergoing surgery to suspend the uterus (and bladder) or undergo hysterectomy. But a pessary may be difficult to hold in place in women who have had a hysterectomy since the walls of the vagina are no longer supported by the uterus and cervix.
Hysterectomy Consequences
Hysterectomy can have serious consequences on bladder and bowel function and increase risk for future surgeries, but the research is mixed, primarily due to differences in methodology. Pelvic organ prolapse is also a possibility. Important variables that increase or decrease the risk for future problems include the reason for the hysterectomy and pre-operative bladder and bowel function. If endometriosis, fibroid or other conditions compromise or affect bladder and bowel function pre-surgery, then odds are they will be affected post-surgery and whether there is improvement or further damage depends upon a number of factors, including the surgeon’s skill. In contrast, and I think where most women are interested, is whether these problems can arise post-hysterectomy when no such problems existed pre-surgery. The answer is yes, there is an increased risk for both urinary and bowel incontinence post hysterectomy.
Additional Resources
This RadioGraphics article details the pelvic organ sequelae that can be caused by obstetric and gynecologic surgeries and the imaging techniques for diagnosing them.
This Medscape article details the Long-term Effects of Hysterectomy.














I’m with you Jen there is so much negativity surrounding having a hysterectomy but considering the prolapse I carried around for 10 years after having my son, I can’t imagine anything could be worse! To have your uterus and bladder hanging out of your vaginal opening every day was the WORST!!! I considered a pessary but seriously having to take it out and put it back in again for the next 40 odd years, no thanks! I’m in Australia and we have an amazing hospital and health care system and I have full faith in my urogynocologist that she advised me correctly and I have had a full hysterectomy almost a week ago. It was a vaginal hysterectomy and I was up and walking around the next day. I initially used movicol to soften the contents of my bowel and had my first, very easy bowel movement 3 days after surgery and was allowed to go home. I’m not in any pain other than a feeling of “heaviness” and slight ache but that’s to be expected less than a week post surgery. I’m uruinating without any issues either and although I wasn’t incontinent prior to surgery, my bladder was already partially hanging out of my body so had to urinate more frequently. I have retained my ovaries so that I continue to produce hormones as I should to take me through peri-menopause as I’m 48. At this point in time I have absolutely no regrets about having the surgery and I suppose time may tell and things could change but at this point in time having a vaginal vault rather than the prolapse I’ve lived with for the past 10 years is the best outcome I could have hoped for and yes it’s possibly early days yet but so far everything is functioning as it has or should and I’m amazed at how quickly I’m recovering and the extent of my mobility already!
Yes it’s great to hear from other women’s experiences but every comment seems to be very “anti” would be nice to have some responses from the other side who have experienced success and relief, unless at some point every person who’s had a hysterectomy ends up.wuth issues?? But isn’t age also a factor along with muscle strength and collogen production when it comes to prolapsed and the dropping of organs such as the bladder in women over a certain age?????
I had hysterectomy in 2014 when i was 50, removed uterus and cervix. I had excessive fibroids at that time was having unbearable pain in my back, constipation etc. The doctor said there was no alternative solution other than this as fibroids had overgrown my whole uterus inside and outside. He said it was like a cauliflower and normal uterus weighing 0.4 kg had become 1.5 kg at that time. 4-5 years after surgery i was feeling great. Than my UTI got worse, having 2-3 times a year and vaginal fungal infections and bowl irregulatories etc. I have vaginal dryness as well. Dr 2 years ago prescribed vaginal estrogen inserts. It helped at the beginning and now i feel it doesn’t help anymore. I have also bad insomnia problem mood swings i feel i am overly sensitive and getting more angry everyday. Last time i visited her she gave me progesterone.
Each time i have uti i take antibiotic but than leaves to vagina discomfort and get anti fungal one dose antibiotic. This time even after that treatment i am still not 100% comfortable and frustrated of all going on. I have been searching for a while what the problem is. Is it urinary problem or pelvic floor problem.
Julia, I’m sorry you are dealing with all these after effects. It seems that using the vaginal estrogen several times a week would prevent the infections. D-mannose, a supplement, is supposed to be helpful for preventing UTI’s. Here’s one study – https://europepmc.org/article/med/27424995. Also, your other symptoms are indicative of impaired ovarian function.
I had a daVinci laparoscopic assist vaginal hysterectomy. I am 8wks post op. Mine was due to excessive bleeding.
Artificial hormones cause me heart issues. Ablation can fail or the scarring can cause difficulty in determining future cancer detection; my family history is such that ablation is not worth the risk. So- hysterectomy was my only option.
I have never had bowel issues before the surgery. It took me 15 days to have a BM after surgery, and that was by doing an enema. Ever since surgery, I do not have a BM. Ever. Every 7-10 days, after I’m totally miserable, I have to force it with copious amounts of laxatives and enemas. Dr finally had me do magnesium citrate in the hopes it would jumpstart my system after a full clean out. I didn’t go again for another 8days until I did a triple dose of milk of magnesia.
I don’t know what else to do. Everyone says things are fine. CT came back clear. Ultrasound shows full bowels, but no blockage. Dr said everything looked fine during surgery.
Literally the only thing I’ve done differently is have the hysterectomy. I’m starting to question which is worse… hemorrhaging for 3.5wks out of every month, or not being able to have a BM on my own anymore.
Heather, I’m sorry you are dealing with this. Bowel issues, especially constipation, are a fairly common problem after hysterectomy. Hopefully, your bowel function will improve as you get further out from surgery.
It’s troubling that gynecologists fail to inform women of the many negative effects of hysterectomy as well as all available less drastic treatment options such as non-hormonal tranexamic acid for heavy bleeding or watchful waiting for symptomatic fibroids, etc.
I regret my hysterectomy. I was 45, and was experiencing issues with uterus. Now I have very little muscle control. I have close calls with bladder issues. Overall, sex is no longer satisfying, as I basically just feel like a big hole.
Brenda – I am so sorry that you were also a victim of the hysterectomy industry. Gynecologists need to be held accountable for all the women they harm. It would be great if you would tell your story as part of the HERS Foundation’s “In My Own Voice” – https://www.hersfoundation.org/in-my-own-voice/. Accepted formats are video, audio or written. I wish you the best going forward.
I had a hysterectomy 3 years ago, both my children were born by Caesarean section, endometriosis, cancer cells & tissue were removed through my abdomen. My abdomen has multiple scars on it and with that came scar tissue that had taken over, grown around multiple organs and was attached the inside lining of my abdomen along with the endometriosis being back. My monthly cycle was so bad I was taking the largest Pads made, putting two at a time in my panties and still changing them every 10 minutes for 5 days out of a month. That changed and started happening to me 3 weeks out of a month. I have always been anemic, started having kidney stones at age 3. The hysterectomy conversation started with me at age 16.. I managed to hold on to everything until I was 40, but the cancer & the scare of breast cancer plus my mom, my sister & my grandmother had already fought all of it I agreed to the hysterectomy plus it was an emergency situation. I started hemorrhaging and with everything so close together plus all the extra with the scar tissue & endometriosis, they could not find where the bleeding was coming from so I have a complete and total hysterectomy. I spent the night in the hospital, but when I woke from the surgery my doctor told me he knicked my bladder and I would have to wear a catheter for at least 14 – 30 days for bladder to heal. My bladder had to stay dry in order for it to heal and fluids could not go into it. I told him I understood considering everything he had to go through to do the hysterectomy I am surprised that’s the only damage done. I made it through that. I was amazed at how small my bladder was afterwards, I went to the restroom everytime I drank something, in the process it flushed out the rest of my kidney stones, so there’s the silver lining.. Anyway, presently, I have no kidney stones, I have blood in my urine and it still hurts to have sex. It’s not dry, it’s a sharp, shooting pain almost like he didn’t take something out. The blood in my urine started yesterday and it’s bright red, not from sex, I have not had sex and it’s not kidney stones. My right kidney is damaged but it’s not hurting.
Michelle – I’m sorry for all your problems and suffering. I hope they can figure out the cause of the blood in your urine. Some women who have endo end up having vaginal bleeding after hysterectomy if endo grows back on the vaginal cuff. And women who still have their cervix can have bleeding (sounds like you had yours removed).
I am 3 months post op. I had a full hysterectomy and bladder prolapse repair at the same time. I now have vulvodynia, it’s very painful, no cure only temporary nerve blockers and litocane give little relief. Surgeon says it’s not from surgery. Don’t believe the Dr. it was caused by the trama & nerve severing. Now i’m lost on what to do next?
Angie – I’m sorry you’re suffering from vulvodynia. I’ve heard it can be very painful. 🙁 Many of us have been misled about the need for surgery as well as brushed off and negated when the after effects and complications set in. That seems to be the norm.
Some tmes when I pee it goes slow like it’s not coming out sometimes it ok.
what about hysterectomies that are not abdominal where they only use small incisions
Liz – Hysterectomy causes permanent harm regardless of how it’s done. The uterus is essential our whole lives. Please read all my articles as well as others about hysterectomy. My articles are here – https://www.hormonesmatter.com/author/ws/ and all hysterectomy articles should come up if you follow this link – https://www.hormonesmatter.com/category/womens-health-cat/hysterectomy/.
I started reading EVERYONE post & what they went through before looking at the article. Nothing beats another woman’s experience good & bad.
Thank you to everyone who has shared. I’m still trying to make a decision since I have overactive bladder I do not want to have my situation worse.
Liz – Are you saying your doctor is recommending a hysterectomy for overactive bladder? Is your bladder prolapsed? If it is, a pessary can be used to suspend it, no surgery needed. Unfortunately, many doctors will not even mention this option as it’s not a money maker for them unlike hysterectomy that is their “bread and butter”. There are many types of pessaries and a doctor who knows how to fit them is your best bet if this is your problem.
But regardless of your problem if you do not have cancer, a hysterectomy is probably totally unnecessary. Trust me, it causes more problems than it fixes especially in the long-term.
Please post back to explain further. Thanks.
When I read some of these comments it really saddens me. A hysterctomy is not the answer for everyone. I had a complete hystorectomy two years ago….and I have had NOTHING but problems..never had urinary problems until after the surgery. Stand up out of bed, I have to hold tissue their so it won’t leak out., bleeding after sex, don’t have that anymore..now I have pressure in my Virgina area…can’t go to the bathroom..am constipated..take merylax everyday to relieve the pressure. I feel like a baboon butt….I had the Goldstien bladder mesh put in. I am wondering if it has let go. I was given a hormone cream to insert vaginaly but never used it..I was told it would help when you have entercourse…WHATS THAT ? I am not into pain and bleeding..it’s not a turn on..so I was wondering if anyone else was experiencing this.. Called my doctor ..asked the nurse if it could be the bladder mesh and all she kept saying was use the cream…it’s not the mesh…Ihad no choice from what the doctor said my uterus and bladder had dropped..I was working with a trainer , had three kids natural and she said that didn’t help…I don’t want anymore surgeries…I’ll suffer threw till the end…just more things for them to mess up…HELP …
Val, I’m sorry that you too became a victim of this harmful surgery. Bladder and bowel problems are common after hysterectomy but it’s possible that the mesh is partly to blame. However, surgeons will typically deny that their surgery caused any problems. And other doctors don’t tend to incriminate their peers for poor treatment such as a surgical mishap, misdiagnosis, overtreatment, etc.
Before I had a total hysterectomy..I would read and watch videos like these. This video is way out of porportion to what really happens. I had cancer.
1) My recovery was under a week. In bed one day..no pain..walking around the next. I did need a catheter for a couple of days..due to the anesthesia. I had laparoscopic surgery. I could easily have gone back to work in one week. Never even used the pain pills. Amazing!
2) In fact my bowel function is better now. Maybe because it is not as crowded.
3) yes the vagina is shortened I believe..but that may be due to the pelvic radiation that I had.
Please study your body…but do not let all these scary videos frighten you.
Carol, I’m sorry that you were one of the small percentage of women who had no choice due to cancer. Was your surgery recent? Many of the problems caused by hysterectomy don’t happen overnight. Like you, I had a very easy surgical recovery but the problems that have developed over time have been devastating. As far as the vagina, it has to be shortened to close it off (sort of like a seam that’s needed when making a garment). But yes, radiation can cause further “shrinkage.”
The videos certainly are frightening and many women probably think that a surgery so common could not cause so much damage. But I urge all women to heed them as the uterus is vital for a number of non-reproductive functions. And the many hysterectomy forums are evidence of the problems that ensue.
I wish you the best of health going forward!
I just had a total Hysterectomy on May 17th, 2017. Today I am two weeks post op. I still have pressure and I also feel I have a hard time sitting. When I do I can’t breathe very well my lower back kind of hurts. Is this all normal and I will feel better? Fingers crossed.
Mary, You’re still early post-op. Pain can cause us to not breathe normally. However, having trouble breathing can be indicative of a blood clot. You should contact your doctor’s office.
I had my radical abdominal hysterectomy May 7, 2018. My bladder had adhered to the uterus which had a slow growing cancer that was half way through the uterine wall. I had the ovaries, tubes and 7 lymph glands removed also. I had a serious intestinal blockage which I got rid of by refusing some of the constipating opioids and walking the floor of the hospital until the blockage passed. 10 days after surgery my very long incision opened wide. I don’t know how I did that. I assumed the responsibility of dressing my wound until the entire thing closed up. Very upsetting procedure but I am proud of myself. I had no incontinence now, perhaps because they hung my bladder with a fine netting. I do my pelvic exercises daily. I do cardio also. I’m losing weight too. I thank God and my two surgeons for giving me my life back! I am very positive that I did the right thing. Mind over matter.
Jeannie – I’m sorry you had cancer and then surgical complications on top of it. I wish you the best moving forward after this major surgery.
I had a hysterectomy for my heavy bleeding and a slightly enlarged uterus and I will regret it for the rest of my life. My Dr failed to inform me of all the horrible side effects and now I will live out my life with organ prolapse and all of the other issues that will ensue in the years to come. When I was 48 years old, I had a hysterectomy (in 2010) and then had a sacrospinous ligament suspension in March of 2016 which failed in the first 7 weeks and has left me in pain ever since. My Dr never tested for blood disorder or check hormone levels or anything else. She said that was the solution for me and she must be laughing all the way to the bank. Hystertecomy should be rare and reserved for those have cancer or other situtations that require this typed of debilitating surgery. It is crazy how often this proceduce is performed. There should be a mandatory class or instruction video that details the procedure and the consequences as part of the informed consent process so that all women are informed completely! They call this modern medicine – I don’t think so.
CW, I’m SO sorry this was done to you too. Thank you for sharing your story.
I totally agree the doctors should give us all the reasons not to have one especially if there is no cancer!
Informed consent, emphasis on informed. The risk/benefits balance is partly unpredictable in the long run. We make the best decisions we can, given our circumstances, but more information should be readily available. And, in the 21th century, hysterectomy should not be the only diagnostic tool for uterine cancer if the D&C is inconclusive.
Lisa, I’m happy to hear you are having no problems post surgery. I’m 12 years post op and I too felt great and like a new woman for about the first 2 years but that all changed and I’ve had 2 surgeries since, to tack up my bladder. I stay fatigued and have no sexual drive and depression from all of that is an UNDERSTATEMENT! I wish you and all you ladies the best.
I had a partial hysterectomy 8 months ago I had a laparoscopic and vaginally, the day I came home from surgery I felt pelvic pain and pain when I am emptying my bladder. My doctor thought it was a UTI which is common after surgery but it was not. When I went in for my 6 weeks check up I told my doctor I was still having pelvic pain and pressure and pain when I empty my bladder. She told me it was normal and then I should go back to work and by moving around it will get better. After 1 month she finally referred me over to a urologist at first they diagnosed me with intestinal cystitis but I know that wasn’t the symptoms I was having, I had so many tests done in the meanwhile I was still having the pain then when my urologist did all the testing and everything came back normal he didn’t know what the problem I was having so he had to refer me to another urologist get a second opinion. When I finally saw her she diagnosed me with pelvic floor weakness due to my surgery, she stated it was due to the trauma from my uterus coming out through my vagina and it caused my pelvic floor muscles to tighten which is causing the pelvic pain but also my pelvic floor muscles are so weak so she referred me to physiotherapy. I have to be on pain meds during the day and valium at night that I insert vaginally. When I had my first therapy appointment my therapist said she has never had a client that has had pelvic floor weakness due to surgery. She also stated that I am that 1% of this happens to and when she did my biofeedback she said that I was lucky that I am not incontinent because of how weak my pelvic floor muscles are. I have now been doing my therapy for two months and nothing is improving I do home exercises and all it does is trigger my pain. I am currently off of work because I cannot work because of my pain. I’m feeling the frustration and the fear that I’m not going to get better. I just need to know if there’s anybody out there who has experienced the same thing that I am going through. I don’t want to give up hope.
Yolanda, I’m sorry you’re suffering so and pelvic floor therapy is not helping! I know of other women who have had chronic pelvic pain and bladder problems since their hysterectomies. I don’t know if any of them have been diagnosed with a weak pelvic floor. Hopefully, someone will see your comment and have some insight. I hope you’re able to get relief!
Hi,Yolanda I’m sorry to hear about your bladder pain and bladder issues. I’ve had bladder pain and issues myself and I tried the physical therapy for my pelvic floor and it did not help me or make the pain better. Its been three years and I still have bladder pain and pelvic pain. Especially when empty my bladder it is extremely painful. I’m not sure if it’s damage to the urethra and bladder or scar tissue. I know I get very scared at times because I don’t know what’s causing it to be so painful?
Yolanda and Jenn i am so sorry y’all too are enduring this hell! Find a Dr that will listen and assist you…specialty doesn’t matter at this point. Remember you have a choice as to any therapy you do or do NOT want! What’s important is that they listen to you and are willing to work TOGETHER with you; ask questions and listen wholeheartedly. It is possible to have a urethral prolapse…I unfortunately do due to my severe constipation. It ruptured/my sling busted (?) yet NO ONE will touch me with a 10’ pole. My GI drs have also washed their hands of me and stated I was a very complicated case and beyond what they can do. So the last 5 years have been hell yet now here I stand alive and able to do things with my cancer fighting momma, school aged granddaughter including camping and much more. We did have to purchase an affordable motor home so that I can make a 3 1/2 hour trip. I can’t sit, lie, stand nor walk for too long and have to remind myself “ DO WHAT YOU CAN AND ENJOY THE MOMENT. LIVE IN THE PRESENT….!!” Don’t give up!! Don’t fret too much because it will do you more harm and age you 100,000%….I’m severely obese and I look old. So what I am telling y’all is FIGHT LIKE HELL!!! Give satan the boot because he loves to make you miserable….YOU WILL BE OK, maybe not today nor tomorrow but one day YOU WILL look back and say “ WOW I MADE IT OUTTA THERE…!!” I still have an “80” year old body but It will NOT let it stop me from enjoying my life. Accepting the inevitable has been far easier than fighting the reality of it all. Remember 2 words…Accept it all and change what you can. I had 1 friend that God truly sent my way to remind me all would be well and not sweat the Small stuff….no judgement just unconditional love. So now I am telling you “ BREATHE”, remind yourself “I am alive and this will not kill me…I am ALIVE & WELL, thank you God!” Don’t focus on what you had, focus on WHAT YOU HAVE!!! ?
Hope this helps y’all. There are compounded urethral inserts that have lidocaine, antibiotic, and anti inflammatory…hurts but does help. I struggled in letting my husband do it and finally stopped. I could allow my PT /urologist nurse to insert but it was too expensive. Hycosamine tablets relieve me of spasms and Xanax helps release tension down low. I also used lidocaine vaginally to help with painful sex along with Estrace at bedtime/after intercourse. I also purchased a do at home biofeedback (Intone) device for physical therapy and eventually stopped all therapy. Not smart but due to the pain/depression etc I just stopped. Now I can tell that it was all helping me…everything I stopped doing I realize now I should’ve never stopped. However, I ALWAYS have the option to get my poop together and start again. Baby steps even count in this stage of life…just keep moving and doing the best you can. We are survivors of a hell unknown to many. God bless!
Hi ,I had Hysterectomy 7 years ago and have a good life for 5 years and after all has been changed I am in palvic pain now have back wall prolapse and little bit front I have to do surgery to fix it so stressed about all this happened to me
Elena – I’m sorry you’re suffering from what sounds like vaginal vault prolapse. Be sure to do your research on surgery for this before going forward. I hope all turns out well!
Yolanda, how can i get in touch with u…we are going through the exact same thing and need to talk.
Testing
I have been bleeding for seven Years.I am now 57 and I was on menopause when I was 50. Doctors have told me that there are many polyps inside the wall of my uterus that cannot be removed because the uterus might get ruptured. Many exams show no cancer at all but the risk of hyper plasia is always there since the wall is thickened. I have an appointment for total hysterectomy next month, do you think I should avoid it.
Mah. My uterus was full of cysts. Due to heart issues I wasn’t able to have a full hysterectomy I still have my ovaries. Most of my pain subsided by removing uterus. Just dealing with an ovary that won’t quit hurting now. Get a second opinion if I were you. But I’m glad I had mine out!
Thank you Cathy. Your response was very helpful.
Mah, Have you already had a D&C and polypectomy? Is your uterine lining truly thickened? Fibroids and polyps can make it appear thicker than it is because ultrasound cannot always differentiate the growths from the lining itself. It’s good exams have not shown any signs of hyperplasia or cancer.
Mah, I feel for you with all the bleeding. I had fibroids bad & had a complete vaginal hysterectomy at 56. It’s the best thing I ever did for myself. I would go buckets. I was lucky & had no complications at all & I had an awesome surgeon. But for the last 4-5 years or so, my bladder has come down. It hasn’t come out, but it bothers. It would get painful. So I was reading an article on line last week about using tampons for that. I tried it over the weekend & wa-la. It works! It pushes it back up where it belongs. Not feeling that bulge is wonderful. The article said this can’t hurt you. It’s certainly an answer to my problem. This may be something for others to consider.
Gail, I’m sorry you’ve developed bladder prolapse since your hysterectomy. It sounds like your ovaries were also removed as was the case for many of us. What was your surgeon’s reason for that?
Thanks for sharing this tip. I read somewhere else recently about using tampons as a “pessary.” However, they do have to be removed frequently due to risk of Toxic Shock Syndrome. And since they’re absorbent, a water-based lubricant should be used with them. I wonder if a re-usable menstrual cup would be a better “make shift” pessary since they don’t have to be removed as frequently. Of course, since they lack absorbency it may be harder to keep them in place. Just a thought…
Can I call you for a consultaion?
Mah, I do not counsel women about hysterectomy but you can read all my articles here along with women’s (and some men’s) comments – https://www.hormonesmatter.com/author/ws. You can contact The HERS Foundation to request a consultation – http://www.hersfoundation.com/contact.html. Best of luck to you!
Thank You.
Two years post complete hysterectomy at age 70 to remove pineapple size fibroids and I wish I had done my homework first. Constant severe cramping and bloating…worse than before my surgery. I’ve had two pelvic sonograms and Dr say everything is normal I hate when they act like its all my imagination..
Shirley, I’m sorry you also regret having had a hysterectomy. Many women complain of bloating. It’s not surprising since our pelvic anatomy is altered – cutting of blood vessels and nerves, displacement of bladder and bowel and possibly other organs. Thank you for sharing your experience.
Is there anything we can do to help with the appearance of the belly?? My stomach sticks out like I’m pregnant since my hysterectomy. I hate it
Marcy, I hate the disgusting big belly too! I don’t think there’s anything we can do. Our spine, hips and rib cage have been displaced. I used to be able to wear form fitting clothes but avoid them now. I hate mirrors! How long ago was your surgery?
This article seems to be highly anti hysterectomy. I had constant blood cyst in the left ovary and over 40 fibroid cyst on my uterus. Removing all 40 plus was not an option because more would come back not to mention it is not practical to continue to remove blood cyst surgically. I am 3 weeks post op and have more energy now then before. I am also no longer in searing pain. I am only having constipation…which is how I found this article. I can deal with that better then constantly being in pain. I have spoken to several women who are several years out and they all said it was the best thing they have done. So I am wondering about the negative tone of this article. Again constant surgery to remove over 40 fibroid cyst that keep returning, constant surgery to remove growing blood cyst is not only impractical but extremely expensive. Also I had adenomyosis. A very painful disorder that is not curable. This article speaks negative about hysterectomy but does not touch on the negative side effects of birth control…which don’t go all female issues. So any ladies who are considering hysterectomy please research and look at cited works. Do speak to others and don’t be scared by biased sources.
Jen, I’m sorry your gyn problems led to hysterectomy. The after effects of hysterectomy detailed in my articles are supported by medical literature for which I included citations. The problem is that most gynecologists fail to fully inform their patients. I only hope that women find my articles before having a hysterectomy (and/or oophorectomy) so they can make a FULLY INFORMED decision.
Yes I was lied to my life was ruined at 28 I was told the dr would fix my prolapse, I would be able to continue to breastfeed, my anemia, would get better because the bleeding would stop, no more pain from rupturing cysts, or painful intercourse. He hit my bladder with a robot arm, destroyed my vagina, I weigh 84 pounds now, my epilepsy was so minor it wasn’t even worth getting diagnosed hormones going wild and utis have made me have several siezures daily now, I have to use catheters for the rest of my life. I need reconstructive surgery to fix what he did, but no dr will take on his complications so he has effectively barred me access to gyn care. I still have endometrial implants, I have no idea the amount if damage he caused to my intestines and may never know, and terrible scarring. Nothing got better I can no longer work and I have osteoporosis I have spent 32 days in the hospital since my surgery less than 2 yrs ago. My sister had the same surgery with a different surgeon around the same time and her bladder actually ruptured her’s could be fixed through multiple surgeries but it will never be the same. The uteran prolapse incontinence is nothing compared to the pain of a neurogenic bladder. They shove papers in your face and lie to you to get you to sign them don’t do it. Both my sister and I were told to pretty much give up on malpractice cases. Crazy right, this is actually common and no one cares. Unless you will die without it don’t do it, I was pretty close to that point myself when I made the decision but I wish I would have tried every other option available, now I’m almost bedridden at a few weeks from 30.
Jade, How horrific! I’m so very sorry this happened to you! The greed in medicine and especially in the Gynecology specialty is out of control. And it continues to shock me that no one is doing anything about it. Robotics has made it all worse since the costs of those expensive machines have to be recouped. The inadequate training and use of the robot when it isn’t appropriate puts women at further risk for injuries.
With your debilitating injuries and young age, it’s shocking that no lawyer will take your case. I think some states have a 1 year statute of limitations which is ridiculous but I thought most have a 2 year statute. Have you tried your state’s Bar Association for referrals? The non-profit HERS Foundation may be able to suggest some or offer some guidance on finding one. You can contact them via a form on their website or by phone – http://www.hersfoundation.com/.
Regardless of whether or not you get someone to take your case, it would be a good idea to file a complaint with your state’s medical board and also your insurance company that authorized the surgery (assuming you had insurance).
Interestingly, I did read the other day that antibiotics can increase seizure risk so it makes sense that treatment for UTI’s could worsen your mild epilepsy. It sounds like you had discovered this.
I wish you the best in getting help with all of this!
You mentioned about issues with your bladder during surgery. I went in for a tubal ligation and the ob punctured a hole in my uterus…I still have everything. But I have been diagnosed with endometriosis, pcos, pelvic organ prolapse, pelvic floor dysfunction, interstitial cystitis, ibs-c, and I have multiple ovarian cysts that keeps rupturing. I live in constant pain and can’t work. I still have my uterus and ovaries…
Dana – I’m sorry that you too were harmed by a gynecologist. Although tubal sterilization procedures are common, they too have negative after effects as well as possible surgical complications despite what women are told. And those that use Essure coils have been shown to be even more problematic (don’t know if this is the case for you).
How can it be for or against hysterectomies Jen when its just women sharing their stories. Isn’t that the purpose of this site?
I’m ten years post opt. I just want to say – 2nd and third opinions and pray. I don’t think I’d do it again. No. I know I would opt for a different route because my L5 vertebrae is now sitting on my tailbone and my issues are just changed. God’s discernment for you all!
Kelly, I’m sorry you’re also suffering the negative effects on your spine! I haven’t had any x-rays but my back and hips do tend to get sore. I’m also 10 years post-op from this awful surgery! I hope you can find something to help! Thank you for posting.
I am 2 wks post-op and it hurts when i go pee so bad,even my rectus hurt. Is that normal. My dr. did not explain nothing to me.Is so deppressing
Ciara, I’m sorry your doctor wasn’t forthcoming; most aren’t when it comes to hysterectomy. You may have a Urinary Tract Infection (UTI). Those are pretty common after this surgery. Please see your doctor / surgeon.
What a negative article.
There are many negative after effects of hysterectomy since the uterus and ovaries are essential our whole lives. You can read the rest of my articles by clicking on my author name (WS) at the top of this article. The HERS Foundation’s Female Anatomy DVD is also a good resource. Did you have a hysterectomy?
Elizabeth, I couldn’t agree with you more. I can’t decide if she was just so sad to loose her uterus or if she just wanted other women to feel just as miserable.
Venita, Did you have a hysterectomy and what prompted you to go in search of articles on this subject? Women who are happy with the results generally don’t go in search of information.
Please stop. Downplaying other people’s experiences just because they are different from yours is not helpful. Plus, you’re coming across as just plain rude.
Many of us were singing the praises of our hysterectomies for the first 2-4 years–then something changes (like the pelvic floor weakening) and serious, serious debilitating issues begin. NONE of the potential consequences of having a hysterectomy at 35 were explained to me and all my questions were brushed aside. The experiences being shared here are vital to helping other women make an informed decision. I WISH I had seen more stories like this before I chose to have mine for severe endometriosis, fibroids and cysts. I kept one ovary-which lasted less than a year. A very large hemorrhagic cyst ruptured and took my ovary with it. The internal bleeding was so severe that I was going into shock and had emergency surgery and a transfusion. They siphoned more than 2 liters of blood from my abdomen. I almost DIED that night. Now my pelvic floor is extremely weak, my thyroid is a wreck, my hormones are a wreck and I wasn’t told ANY of these were potential consequences. I also have zero sex drive and it breaks my heart because I’m crazy in love and still very attracted to my husband and miss sex!!! I would give anything to go back and change my mind. I wish I had gotten second and third opinions and visited an endometriosis specialist before I made my choice. Now I can only hope that this helps someone else.
So please, please stop trivializing and dismissing the negative consequences of hysterectomies because YOU haven’t experienced them. Just consider yourself very lucky and pray you don’t wake up one day and find yourself joining our ranks.
Thank you for your comments, as I read them I’ve been considering both procedures to resolve my issues, however it seems they may only cause more. It’s really important to get both sides to help women make informed decisions. Everything has side effects it’s just about working out what you feel is best for you.
I started reading EVERYONE post & what they went through before looking at the article. Nothing beats another woman’s experience good & bad.
Thank you to everyone who has shared. I’m still trying to make a decision since I have overactive bladder I do not want to have my situation worse.
I am so sorry that invasive surgery and incomplete informed consent are STILL so prevalent in 2016. I found this forum as I have been having heavy vaginal bleeding that resulted in extreme anemia, (hemocrit of 4.3. I was about to have a heart attack), and after that crisis was resolved with a blood transfusion, my doctor’s first response was, “well why don’t you just have everything removed?” Um, because I am 53 years old and unless I have cancer, this should resolve itself pretty soon! I am on progesterone now and my bleeding is down to just a smear. The cramps are terrible, but after reading about the debilitating pain that others have experienced after botched ablations, I think I am doing just fine!
Women in my family have a history of having one looong laaast period to end menses. This is actually pretty common, but not something you often hear about. And it really freaks doctors out! It is amazing to me that so many doctors are so ill-informed about Change of Life matters! My mother was very open about what she experienced during her menopause because she wanted to be sure that no other women in our family suffered like HER mother did because of a medically unnecessary hysterectomy.
My grandmother had a hysterectomy sometime in the mid to late 60’s because she had an enlarged uterus. She had already undergone menopause. She had had five children and five vaginal births. Although she was slightly overweight before the surgery, after the hysterectomy she rapidly gained weight. She was, at most, 5’3″ but probably weighed 300 pounds. I do not know when her complications set in because she did not talk about her experience until shortly before her death in 1991, but she apparantly experienced all the horrors of pelvic organ prolapse. Even though I was young, I remember that she had multiple bladder stapling surgeries, one of which I swear was reported to have been to staple it to her backbone! (But I was VERY young and may have misunderstood. There isn’t anyone left to ask.) What she didn’t confess until years later was that her doctor, frustrated by these many surgeries on what he considered to be just some ancient, obese woman, decided that the best way to treat her organ prolapse, pelvic floor problems, incontinence, etc., was to sew up her vagina! He did not discuss this with her beforehand. She awoke from surgery to find that her doctor had been unable to do another bladder stapling and he solved his problem by sewing her up! He didn’t think this should be a problem since she was a widow. She wasn’t using it anymore, so what’s the big deal? My grandmother was, at most, 65 years old! My grandfather had only been deceased a year or so. This doctor should have been drummed out of the AMA!
My grandmother’s debacle happened in about 1972. She was so humiliated by it that she didn’t speak about it for nearly 20 years. I can only hope that her doctor now has his own special little corner of hell, or has been reincarnated as a woman with a high sex drive and gyno problems! As I stated, my mother was so appalled that she probably overshared her own menopause experiences, but at least I knew that for MY family, I was perfectly normal, and I knew to run from that ER doc that wanted to eviscerate me!
My heart goes out to everyone who has been harmed by misinformation and the medical community’s race for the almighty dollar at the expense of patients’ health. I thank everyone who has posted about their adverse side effects, and especially the experts who have shared their knowledge of how and why adverse effects might happen. An edometrial ablation was suggested after I flatly rejected the hysterectomy. After reading about them on WS’s other post, I don’t think I am a good candidate, but I seriously doubt my doctor will concure. Whatever. She can’t touch me without my consent!
Julie, Thank you for posting. I’m sorry for your doctor’s suggestion that you just have everything removed! When I was told I needed my organs removed, I wish I’d responded with “I’ll have mine removed after you have yours (prostate and testicles) removed!” If we could blame it all on doctors’ ignorance about the transition to menopause, it would be one thing but gynecologists are supposed to be the experts on these matters and have plenty of patients from which to learn. It’s much more about the lucrative business of hysterectomy and possibly some need to exert power / control as well.
It’s good your mother was open about the effects of hysterectomy on her mother. Too many women are mum putting so many of us at risk especially since half of women are offered a hysterectomy. It’s no wonder your grandmother’s uterus was enlarged…she had five children! It sounds just as idiotic as the woman whose doctor said he removed her ovaries at the time of hysterectomy because they were shriveled up. That’s what they do as we transition to menopause…they shrivel up like our skin! And there’s a reason for it. The outer part (the theca) is responsible for the reproductive (exocrine) functions while the inner part (the inner stroma) performs the post-menopausal (endocrine) functions.
Of course pelvic organ prolapse (POP) risk increases after hysterectomy since the uterus is no longer there to hold the bladder and bowel where they belong. And the vagina no longer has the uterus and the four sets of ligaments to keep it suspended. It is sewn shut like a pocket with nothing to hold it in place causing it to collapse over time (sort of like a crumpled up shirt sleeve). Ironically, most gynecologists recommend hysterectomy for pelvic organ prolapse versus suspending the uterus along with the other organs! I suspect because it is easier and more profitable! I recall an acquaintance talking about her grandmother’s many prolapse surgeries since her hysterectomy and how they could no longer do anything to keep her organs in her body! Sickening and frightening!
Unfortunately, there are far too many gynecologists like your grandmother’s… performing procedures that do much more harm than good.
I’m so glad you knew to run from the ER doctor and that it’s best to let nature take its course! I’m glad you came across my ablation article too. Being that you are 53, this should all be over soon.
Thanks again for posting and best of luck with getting into menopause without too much angst!
Hystotectomy in 2007. Chronic constipation ever since. Now laxatives aren’t even workin. Severe fatigue, bloating, pain under rib. No answers. This seems to be a common problem yet we can’t find help. My life has been horrible since. Does anyone know what kind of Doctor to see?
Sue, I’m sorry your life has also been “horrible” since your hysterectomy. 🙁 My surgery was shortly before yours (2006) and my bowels have been screwed up ever since not to mention a long list of other awful effects. I’ve had some testing done by a gastroenterologist but still no answers and I don’t think I want to do any further testing.
This harm to so many women needs to be exposed in the media. ProPublica is doing a hysterectomy survey. It can be found here – http://propub.li/1t6uZNr. Although the main focus seems to be on surgical complications, please be sure to include all the effects you’ve experienced since the surgery. This is another way to report your patient harm to ProPublica – https://www.propublica.org/getinvolved/item/have-you-been-harmed-in-a-medical-facility-share-your-story
Consumers Union (part of Consumer Reports) also has a Patient Safety arm. You can report your harm here – http://safepatientproject.org/share-your-story. I reported my unwarranted hysterectomy and oophorectomy in two categories, Doctor Accountability and Medical Errors (even though my organs were intentionally removed).
Best of luck to you in getting some help for your bowel problems!
Yes, I know this is an older post but just in case…
This is what I would do (did)–first go to a GI specialist, a reputable one, and ask about Amitiza or Linzess. They are very good drugs and work differently than what is available OTC. They’ll probably want to do a colonoscopy too–but everyone should have one and colon cancer is fast becoming more and more common among young and very healthy people. Also, check into a women’s center that specializes in pelvic floor dysfunction. Then research their suggestions. Ask about physical therapy/biofeedback.
My name is Tameka and I just had an abdominal hysterectomy last week with ovaries still in place. My problem is that I haven’t had a bowel movement in a week. I feel it piling up towards my vottom. I keep getting the urge to push out but can’t. I’m so scared I may bust somethg straining. It seems as though my hemorrhoids are acting up and there’s no way to get tht first plug out. I’m taking stool softeners twice a day along with using hemorrhoid cream but nothing is working. I told my dr and the ofc keeps telling me to do wht I’m doing. Is there anythg else I can do besides not eat cause I’m tired of this stuff pulling up.
Tameka, That sounds dreadful! Adding a laxative of some sort may help but you may want to check with your doctor. I hope this resolves soon!
Hi Tameka I am 3.5 months post hysterectomy and I have not experienced too many post hysterectomy difficulties. First listen to your body, second Bran buds 1/2 cup daily with milk/or almond milk. Third, light Olive oil 1 Table spoon and drink plenty of cold water until you have a bowel movement. That should do the trick. Keep your body healthy and you should heal well and quickly. But if any serious medical problems arise do not hesitate to call your Dr. immediately.
Hope you feel better. Cindy
Tameka I had the same problem. My doctor sent me home with lactulose and I had to take that for months. I also took gummy fiber to help me out in that area, but it’s still a problem. Prior to my surgery, I had bowel movement two to three times a day every day, but now days go by and I have to try to remember if I did.
Iam 13weeks post hysterectomy and Iam sorry I had it done. I was a very active women, always running around from 6am till 9pm. It has slowed me down Iam incapable of standing for too long and sitting down hurts me as I constantly feel there is something stuck in my rectum. Iam tired all the time. I have the braca 1 cancer gene and have already had two breast cancer. I was advised to have a full hysterectomy wish I just had my overies removed now. As I feel my bowel would still be held in position with the ulterus supporting it.
Joan, I’m sorry you were faced with this decision due to being BRCA1+. And I’m sorry you regret having your uterus removed. I completely understand. I miss my uterus as much as (maybe more than) my ovaries.
I was talked into having my ovaries removed at age 50 after a tiny complex cyst was found on one of them. I still have my uterus. How does not having ovaries effect the organs and pelvic floor? Thanks.
Geri, I’m sorry to hear this! Unfortunately, there are far too many of us who’ve lost organs unnecessarily. It is the uterus and its ligaments that play the key role in the positioning of the bladder and bowel. When those ligaments are cut and the uterus removed, the bladder and bowel are displaced (descend) and no longer have the uterus to separate them. The ovaries’ role is primarily hormonal which can affect bladder and bowel function to some degree. I hope this answers your question.
Thanks for your response! That’s one less thing I have to worry about.
Geri, I reread my first response and realize I didn’t completely answer your question. The uterine ligaments are also the pelvis’ support structures which keep the spine, hips and rib cage where they belong so your figure should not be affected (provided you don’t gain weight) since you still have your uterus. Your vagina shouldn’t collapse either since your uterus and ligaments are intact.
I’ve had pain in my upper stomacher ever science the servery.I had the belly button one done on me.I’ve had like a big rock in my upper ABS but now its huge and I’m bleeding from vagina.I’m so scared.
I am sorry you are experiencing complications. You really need to have this checked out by a doctor. How long ago was your surgery? Please let us know what you find out.
This is the first place I have found a clear full explanation of what my operation was and why I was told no sex for 6 months( after the operation had taken place) a d not 6 weeks as the out of date notes said. i had managed my prolapse with a pessary but realise that this wont be possible if I needed it in the future. Its 3 months since my operation and Ive had a lot of the sude effects described. I also feel as thiugh there is still something dragging dowm. im keeping my hopes up that im wrong but I wish Id had these facts given to me bofire the op!
Jean – I am sorry your doctor failed to tell you the side effects of hysterectomy. For women who want a surgical solution for prolapse, it seems to make much more sense to suspend the uterus (along with the bladder) than to remove it since removal increases risk of bladder and bowel prolapse. Hysterectomy is grossly overused and we are the ones who have to speak out to stop this epidemic harm of women.
I am wondering why the negative narrative about hysterectomy? I am in my third week after open surgical hysterectomy and I am SO glad I did it. For ten years I was slowly dying from large Fibroids and anemia. I feel 100% better than I did before. My sexual function and energy is already better. I do miss my uteren contractions, but now enjoy vaginal ones. I am excited about life again. Sometimes a hysterectomy is a blessing! Thank you.
-Lisa
Lisa – I am sorry you had fibroids. It is a shame that your surgeon did not remove just the fibroids preserving your pelvic and sexual integrity as well as the blood flow to your ovaries. I thought sex was a no-no for at least four weeks post-op since there are a lot of internal sutures that need to heal. Please be sure to follow post surgery instructions for proper healing.
Lisa, in my case it also improved a lot, though I experienced some incontinence for a while. But the improvement lasted exactly three years and since then its got worse and my life is devastated, not only sexually. I am now in the 6th year post.
What can I do to help my fiancée achieve an orgasm due to a vaginal hysterectomy were only the uterus was removed.
Paul – I wish I had some suggestions but I don’t. I hope you and your fiancée can survive the changes. I wish the best for you both.
This is not a pro or con hysterectomy site just a place where women discuss their surgical experiences I thought that this is what its for….