Almost two months ago, Lucine Health Sciences and Hormones Matter started a new research project called the Real Risk Study: Birth Control and Blood Clots. The purpose of this research is to assess the breadth and depth of blood clot risks and other side effects associated with hormonal contraception. We believe that a deeper understanding of medical and lifestyle influences is crucial to providing women with a complete picture of their personal risk for blood clots while taking these medications.
To date we have collected data on 64 to 87 women (depending on which section of the survey we are analyzing) who have suffered from blood clots while taking hormonal birth control. These blood clots include deep vein thrombosis and pulmonary embolism, as well as strokes. Many women in the study have had long lasting effects even after they recover from the initial effects of the blood clot. And some women, unfortunately, have suffered from fatal blood clots, and a family member participated in the study on their behalf.
Risk Based on How Long Hormonal Contraception Has been Used
It is generally thought that the risk of developing a blood clot is highest within the first year of starting or restarting hormonal birth control. However, in a previous article we reported on some of the early data we had obtained, and we found that most of the women in our study had been on hormonal contraception longer than one year when they developed a blood clot. In our current data set, we have data from 87 women, and the same trend continues. Seventy-five percent of women developed clots after the first year on the medication, and only 25% developed clots within the first year. In some cases, women developed blood clots even after up to 21 to 30 years on hormonal contraception.
Risk for Blood Clots Based on Smoking History
One of the goals of the study is to provide a clearer picture of who is at risk for developing a blood clot related to hormonal contraceptive use. In the information provided by pharmaceutical companies, smoking and being over age 35 are highlighted as being risk factors. For example, the package insert for Beyaz/Yaz, the most popular birth control pill in the U.S., states:
Who should not take Beyaz or YAZ?
Do not use Beyaz or YAZ if you smoke and are over age 35. Smoking increases your risk of serious side effects from the Pill, which can be life-threatening, including blood clots, stroke or heart attack. This risk increases with age and number of cigarettes smoked.
In the previous article reporting on some early results of the study, we analyzed data from a question asking women whether they were smokers when they developed a blood clot. Using data from 87 women, the trend previously reported from our smaller data set was borne out again in a larger data set. Ninety-four percent of women in our study were not smoking at the time of the blood clot, and 78% had never been smokers. So although smoking does increase the risk, not smoking does not mean you are not at risk.
Risk for Blood Clots Based on Genetic or Acquired Blood Clotting Disorders
It is known that having a blood clotting disorder significantly increases the risk of developing a blood clot while on hormonal contraception. These disorders can be genetic, meaning that they are encoded in the genes and the person is born with them, or acquired, meaning that they are a result of an environmental factor occurring during a person’s life, such as a drug exposure or another disease. With genetic blood clotting disorders, there may also be a family history of blood clots in other relatives. Genetic disorders include Factor V Leiden mutation, protein S deficiency, and prothrombin mutation. Acquired disorders include antiphospholipid syndrome, hyperhomocysteinemia (which may also be present as a result of MTHFR mutation), and heparin-induced thrombocytopenia.
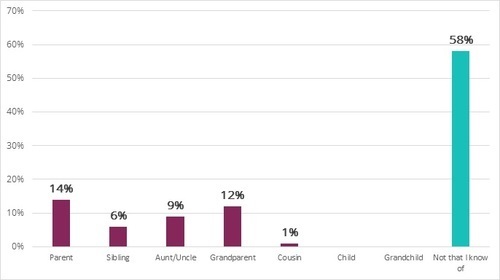
We asked if study participants had a family history of blood clots, and if so, which relative had a blood clot. Fifty-eight percent of the women in our study had no family history of blood clots, and therefore, no reason, from a family history perspective, to suspect they would be at increased risk for a blood clot. In participants for whom there was a family history, parents and grandparents were the most common relatives to have had blood clots, at 14% and 12% respectively. Less common was a history of blood clots in an aunt or uncle, sibling or cousin. These results are depicted in the bar graph below. For a parent or grandparent to be the most commonly reported relative with a blood clot is expected, because the risk of blood clots increases with age.
Family History of Blood Clots in Study Participants
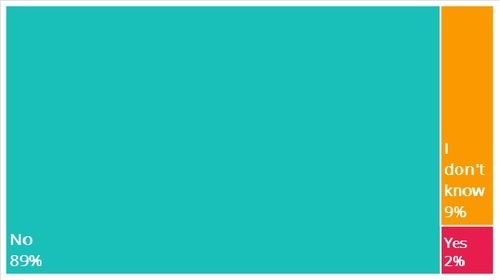
Having a family history of blood clots makes it more likely that there is a genetic disorder that increases the risk of blood clotting running in that family. We asked the women in our study whether they had been tested for blood clotting disorders before starting hormonal contraception. As can be seen below, 89% of the women in our study did not have such testing prior to starting hormonal contraception, and a further 9% did not know if they had any testing. Only 2% of the women were able to state with certainty that they had been tested.
Testing for Genetic Blood Clotting Disorders Prior to Starting Hormonal Contraception
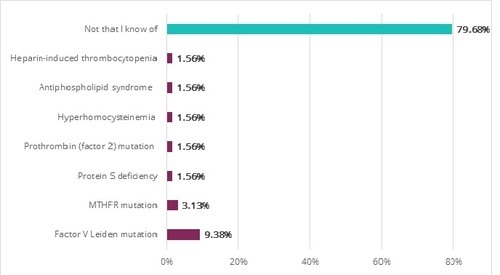
We also asked if the participants if they had a known clotting disorder, recognizing that some women would have been tested for clotting disorders after their blood clot experience, and thus, even if they did not know about a clotting disorder prior to starting hormonal contraception, they may have learned about it afterwards. Only 20% of the women in our study had a known clotting disorder, as can be seen in the chart below. For the other 80% who answered “not that I know of,” it may be that they were never tested for a clotting disorder, or that they were tested and were negative for all known clotting disorders. So far, we do know from follow up interviews with study participants that in some cases, this testing was done and was negative. Upon completion of the study, we will know how many women were definitively negative for all known clotting disorders. Of the 20% of women who did have a known clotting disorder, none were tested for it before starting hormonal contraception.
Study Participants With Clotting Disorders

Of the women that did have known clotting disorders, Factor V Leiden mutation was the most common common disorder, found in approximately 9% of study participants. This is consistent with what is known about Factor V Leiden mutation: it is known to be the most common blood clotting disorder. Other blood clotting disorders were found with low frequency in our study, as can be seen in the bar graph below.
Blood Clotting Disorders Present in Study Participants
Summing Up
So far, our preliminary data suggest that many of our study participants did not have known factors that would increase their risk of developing a blood clot while on hormonal contraception. The majority of women in our study were not smokers, and did not have a known clotting disorder, and a significant number of women did not even have a family history of blood clots. In addition, most women developed blood clots after the first year of medication use. We will be continuing to assess these and other known risk factors as we continue with our study, as well as trying to identify if there are any previously unrecognized risk factors. However, it seems that any woman using hormonal contraception could potentially be at risk. This makes it especially important to learn the warning signs and symptoms of all types of blood clots, and make an informed choice of whether hormonal contraception is right for you, knowing the risks.
Real Risk Study: Birth Control and Blood Clots
Lucine Health Sciences and Hormones Matter are conducting research to investigate the relationship between hormonal birth control and blood clots. If you or a loved one have suffered from a blood clot while using hormonal birth control, please consider participating. We are also looking for participants who have been using hormonal birth control for at least one year and have NOT had a blood clot, as well as women who have NEVER used hormonal birth control. For more information or to participate, click here.